Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan




A fasting glucose blood test measures the level of sugar in your blood after not eating overnight. High results can be an early warning sign of diabetes and may also raise your risk of heart disease.
Chronically elevated fasting glucose is often linked to excess weight, pre-diabetes or diabetes, insulin resistance, poor sleep, or ongoing stress. Understanding your fasting glucose is an important step in protecting your metabolic health and preventing long-term complications.
This guide explains what it is, how it works, what your results mean, and how you can book a comprehensive blood test to check your Fasting Glucose.
Fasting glucose is the amount of sugar (glucose) in your blood after you haven’t eaten or drunk anything (except water) for at least 8 hours. Glucose is the body’s main source of energy, and your levels rise and fall depending on when and what you eat. Measuring glucose in a “fasting state” gives doctors a clear picture of how well your body controls blood sugar without the influence of food.
Think of it like checking the fuel gauge in a car first thing in the morning before you drive—it shows the baseline level your body is running on. If your fasting glucose is too high, it may suggest that your body isn’t using insulin effectively, which could point to conditions like pre-diabetes or diabetes.
Quick facts:
By testing fasting glucose, you can detect issues early and take steps to protect your long-term health.
Fasting Glucose is a key biomarker for metabolic health, acting like an early warning light in your body’s engine. It shows how well your body is controlling blood sugar under baseline (fasting) conditions—before meals influence your levels. This matters because maintaining stable, well-regulated blood sugar is critical to overall health, longevity, and metabolic balance.
When fasting glucose is chronically high, it often reflects insulin resistance — the cell’s reduced ability to respond to insulin. Over time, this dysfunction is a stepping stone toward pre-diabetes, type 2 diabetes, and related conditions like cardiovascular disease, kidney damage, and nerve impairment.
Australia currently faces a growing burden: about one in six adults over 25 are estimated to have impaired fasting glucose (IFG) or impaired glucose tolerance (IGT) — early metabolic warning signs.
Global trends reinforce the urgency: the prevalence of impaired fasting glucose is rising, recently estimated between 5.8% and 9.2% of the adult population worldwide.
By monitoring Fasting Glucose, you can detect metabolic stress early — when lifestyle changes still have maximal impact. Armed with that information, you can take control through diet, activity, sleep and stress strategies to maintain optimal health and longevity.
You may not always notice when blood sugar levels are creeping up, which is why a Fasting Glucose test can be an important screening tool. Consider getting tested if any of these apply:
Regular testing helps detect issues before they become serious, giving you time to make effective lifestyle or medical changes.
When you go for a Fasting Glucose blood test in Australia, here’s what to expect:
You’ll usually be asked to fast (no food or drink except water) for 8–12 hours before the test. This ensures your blood sugar level isn’t influenced by a recent meal. Sometimes your doctor might also ask you to avoid smoking, caffeine or strenuous exercise before the test.
Many people get their fasting glucose measured as part of a comprehensive blood panel (e.g. a metabolic panel, health check, “check-up” bundle). These panels bundle multiple tests (liver, kidney, lipids, glucose, etc.) and spread the cost across them. Some private pathology services let you order panels without a GP referral, then just present the request form at a collection centre.
In short: the Fasting Glucose test is simple, minimally invasive, and widely available. Whether you pay via Medicare or privately depends largely on your referral status and the provider you use.
Your Fasting Glucose results show how well your body is managing blood sugar when you haven’t eaten. A single result doesn’t give the full picture, but it’s an important marker that helps identify whether your glucose levels are healthy, borderline, or high. If your results fall outside the normal range, your doctor may recommend repeat testing or additional markers such as HbA1c, fasting insulin, or triglycerides to confirm what’s happening.
Here’s a simple breakdown:
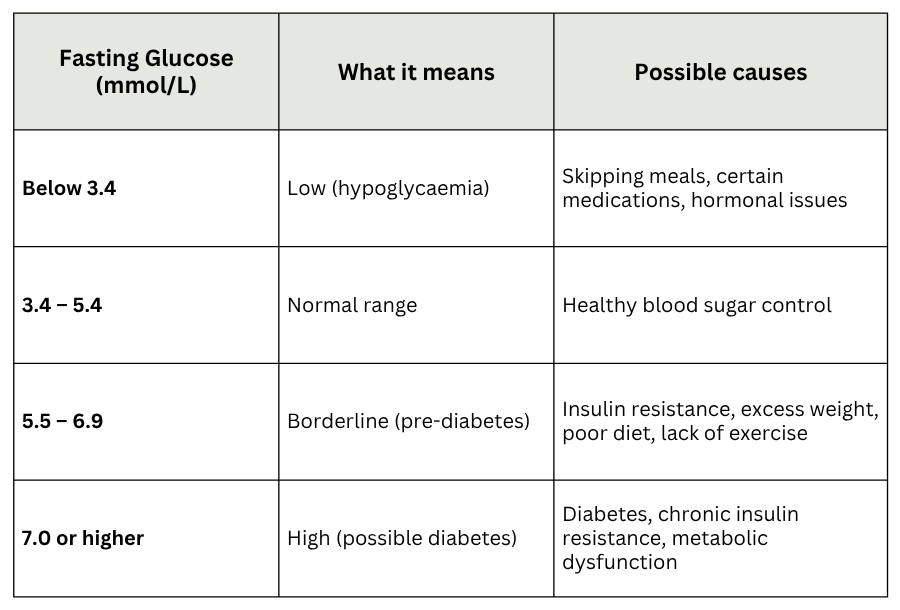
Interpreting these results alongside related biomarkers like HbA1c and insulin gives a clearer view of long-term glucose control. If your results are borderline or high, early action can help prevent complications and support better metabolic health.
A single Fasting Glucose reading is useful, but it doesn’t always give the full picture of your metabolic health. Blood sugar control is complex, and your results make more sense when viewed alongside related tests.
For example, HbA1c shows your average blood sugar over the past 2–3 months, while a fasting insulin test can highlight how hard your body is working to keep glucose stable. Lipid markers such as triglycerides and HDL cholesterol are also closely linked to insulin resistance and cardiovascular risk.
Together, these markers provide a clearer view of your long-term health rather than relying on one number alone.
Looking at fasting glucose in isolation is a bit like checking the weather at one moment in time — it tells you something useful, but combining it with the forecast gives you the bigger picture.
That’s why comprehensive panels that include Fasting Glucose, HbA1c, insulin, and lipid tests are often recommended. Interpreting them together helps you and your doctor spot risks early and choose the most effective steps to protect your health.
Your fasting glucose levels are influenced not only by genetics but also by everyday lifestyle choices. Small, consistent changes can support healthier blood sugar regulation and improve your long-term wellbeing.
The best starting point is testing — once you know your levels, you can take personalised steps.
A Fasting Glucose test measures the level of sugar in your blood after you haven’t eaten for 8–12 hours. It helps detect pre-diabetes, diabetes, and metabolic health issues.
If ordered by a GP and covered by Medicare, many labs bulk-bill, so there’s no cost. Without Medicare, private providers may charge around $30–$60.
Yes, Medicare coverage usually requires a GP or specialist referral. Some private labs allow you to book directly, but you’ll need to pay the fee.
Yes, Medicare covers the test when it’s requested by your doctor as part of routine screening or diabetes monitoring.
Yes. Pregnant women are often screened for gestational diabetes with fasting glucose and other glucose tolerance tests.
You may need testing if you have symptoms such as excessive thirst, frequent urination, tiredness, or blurred vision, or if you’re at risk of diabetes.
Normal is about 4.0–5.4 mmol/L. Results of 5.5–6.9 mmol/L suggest pre-diabetes, while 7.0 mmol/L or higher can indicate diabetes.
Fasting Glucose is one of the simplest yet most powerful markers of your metabolic health. It measures how your body manages blood sugar when you haven’t eaten, providing early insight into risks like pre-diabetes, type 2 diabetes, and cardiovascular disease. Because blood sugar often rises silently, testing is the best way to uncover issues before they affect your daily life.
Understanding your fasting glucose doesn’t just highlight problems — it gives you the chance to take meaningful steps. With the right knowledge, you can improve your diet, activity, sleep, and stress management to better support long-term health and wellbeing.
Knowledge is empowering, and every test is an opportunity to take control of your future health.
Want clearer insight into your blood sugar control and long-term metabolic patterns? Start your Full Body Health Check today and explore over 80 markers.
Subscribe to our newsletter & join a community of 20,000+ Aussies

A fasting glucose blood test measures the level of sugar in your blood after not eating overnight. High results can be an early warning sign of diabetes and may also raise your risk of heart disease.
Chronically elevated fasting glucose is often linked to excess weight, pre-diabetes or diabetes, insulin resistance, poor sleep, or ongoing stress. Understanding your fasting glucose is an important step in protecting your metabolic health and preventing long-term complications.
This guide explains what it is, how it works, what your results mean, and how you can book a comprehensive blood test to check your Fasting Glucose.
Fasting glucose is the amount of sugar (glucose) in your blood after you haven’t eaten or drunk anything (except water) for at least 8 hours. Glucose is the body’s main source of energy, and your levels rise and fall depending on when and what you eat. Measuring glucose in a “fasting state” gives doctors a clear picture of how well your body controls blood sugar without the influence of food.
Think of it like checking the fuel gauge in a car first thing in the morning before you drive—it shows the baseline level your body is running on. If your fasting glucose is too high, it may suggest that your body isn’t using insulin effectively, which could point to conditions like pre-diabetes or diabetes.
Quick facts:
By testing fasting glucose, you can detect issues early and take steps to protect your long-term health.
Fasting Glucose is a key biomarker for metabolic health, acting like an early warning light in your body’s engine. It shows how well your body is controlling blood sugar under baseline (fasting) conditions—before meals influence your levels. This matters because maintaining stable, well-regulated blood sugar is critical to overall health, longevity, and metabolic balance.
When fasting glucose is chronically high, it often reflects insulin resistance — the cell’s reduced ability to respond to insulin. Over time, this dysfunction is a stepping stone toward pre-diabetes, type 2 diabetes, and related conditions like cardiovascular disease, kidney damage, and nerve impairment.
Australia currently faces a growing burden: about one in six adults over 25 are estimated to have impaired fasting glucose (IFG) or impaired glucose tolerance (IGT) — early metabolic warning signs.
Global trends reinforce the urgency: the prevalence of impaired fasting glucose is rising, recently estimated between 5.8% and 9.2% of the adult population worldwide.
By monitoring Fasting Glucose, you can detect metabolic stress early — when lifestyle changes still have maximal impact. Armed with that information, you can take control through diet, activity, sleep and stress strategies to maintain optimal health and longevity.
You may not always notice when blood sugar levels are creeping up, which is why a Fasting Glucose test can be an important screening tool. Consider getting tested if any of these apply:
Regular testing helps detect issues before they become serious, giving you time to make effective lifestyle or medical changes.
When you go for a Fasting Glucose blood test in Australia, here’s what to expect:
You’ll usually be asked to fast (no food or drink except water) for 8–12 hours before the test. This ensures your blood sugar level isn’t influenced by a recent meal. Sometimes your doctor might also ask you to avoid smoking, caffeine or strenuous exercise before the test.
Many people get their fasting glucose measured as part of a comprehensive blood panel (e.g. a metabolic panel, health check, “check-up” bundle). These panels bundle multiple tests (liver, kidney, lipids, glucose, etc.) and spread the cost across them. Some private pathology services let you order panels without a GP referral, then just present the request form at a collection centre.
In short: the Fasting Glucose test is simple, minimally invasive, and widely available. Whether you pay via Medicare or privately depends largely on your referral status and the provider you use.
Your Fasting Glucose results show how well your body is managing blood sugar when you haven’t eaten. A single result doesn’t give the full picture, but it’s an important marker that helps identify whether your glucose levels are healthy, borderline, or high. If your results fall outside the normal range, your doctor may recommend repeat testing or additional markers such as HbA1c, fasting insulin, or triglycerides to confirm what’s happening.
Here’s a simple breakdown:
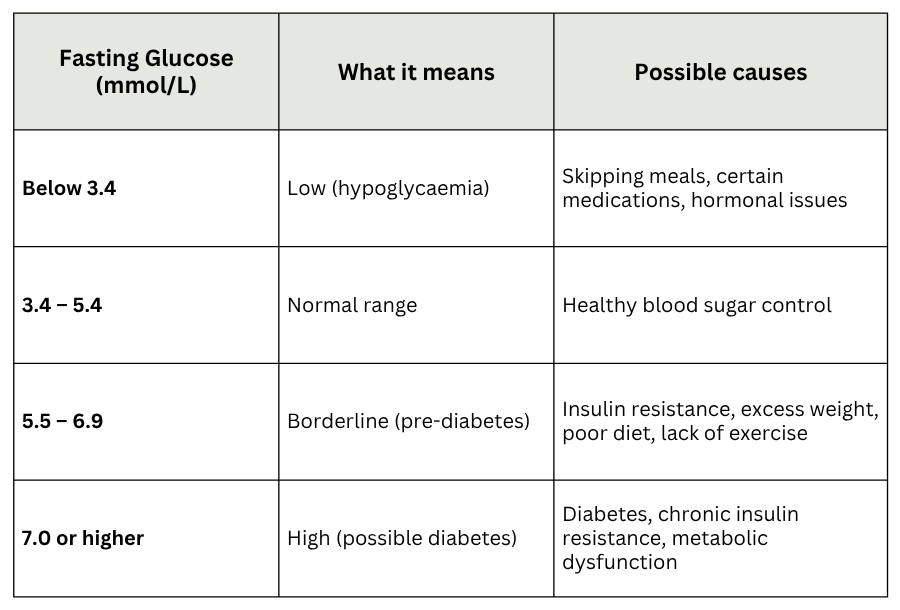
Interpreting these results alongside related biomarkers like HbA1c and insulin gives a clearer view of long-term glucose control. If your results are borderline or high, early action can help prevent complications and support better metabolic health.
A single Fasting Glucose reading is useful, but it doesn’t always give the full picture of your metabolic health. Blood sugar control is complex, and your results make more sense when viewed alongside related tests.
For example, HbA1c shows your average blood sugar over the past 2–3 months, while a fasting insulin test can highlight how hard your body is working to keep glucose stable. Lipid markers such as triglycerides and HDL cholesterol are also closely linked to insulin resistance and cardiovascular risk.
Together, these markers provide a clearer view of your long-term health rather than relying on one number alone.
Looking at fasting glucose in isolation is a bit like checking the weather at one moment in time — it tells you something useful, but combining it with the forecast gives you the bigger picture.
That’s why comprehensive panels that include Fasting Glucose, HbA1c, insulin, and lipid tests are often recommended. Interpreting them together helps you and your doctor spot risks early and choose the most effective steps to protect your health.
Your fasting glucose levels are influenced not only by genetics but also by everyday lifestyle choices. Small, consistent changes can support healthier blood sugar regulation and improve your long-term wellbeing.
The best starting point is testing — once you know your levels, you can take personalised steps.
A Fasting Glucose test measures the level of sugar in your blood after you haven’t eaten for 8–12 hours. It helps detect pre-diabetes, diabetes, and metabolic health issues.
If ordered by a GP and covered by Medicare, many labs bulk-bill, so there’s no cost. Without Medicare, private providers may charge around $30–$60.
Yes, Medicare coverage usually requires a GP or specialist referral. Some private labs allow you to book directly, but you’ll need to pay the fee.
Yes, Medicare covers the test when it’s requested by your doctor as part of routine screening or diabetes monitoring.
Yes. Pregnant women are often screened for gestational diabetes with fasting glucose and other glucose tolerance tests.
You may need testing if you have symptoms such as excessive thirst, frequent urination, tiredness, or blurred vision, or if you’re at risk of diabetes.
Normal is about 4.0–5.4 mmol/L. Results of 5.5–6.9 mmol/L suggest pre-diabetes, while 7.0 mmol/L or higher can indicate diabetes.
Fasting Glucose is one of the simplest yet most powerful markers of your metabolic health. It measures how your body manages blood sugar when you haven’t eaten, providing early insight into risks like pre-diabetes, type 2 diabetes, and cardiovascular disease. Because blood sugar often rises silently, testing is the best way to uncover issues before they affect your daily life.
Understanding your fasting glucose doesn’t just highlight problems — it gives you the chance to take meaningful steps. With the right knowledge, you can improve your diet, activity, sleep, and stress management to better support long-term health and wellbeing.
Knowledge is empowering, and every test is an opportunity to take control of your future health.
Want clearer insight into your blood sugar control and long-term metabolic patterns? Start your Full Body Health Check today and explore over 80 markers.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
