Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan




An eosinophils blood test measures the number of eosinophils, a type of white blood cell that helps fight parasites and is active in allergic conditions like hay fever, asthma, and other immune reactions.
Elevated eosinophil levels are often linked to allergies or parasitic infections. While not directly tied to weight, ongoing allergic inflammation or parasitic illness can affect digestion, energy, and overall wellbeing. Understanding your eosinophil count provides important insight into immune function and potential underlying health issues.
This guide explains what it is, how it works, what your results mean, and how you can book a comprehensive blood test to check your eosinophils.
Eosinophils are a type of white blood cell that play a key role in your immune system. Think of them as your body’s “allergy and parasite fighters.” When the body detects certain triggers—like pollen, dust, or parasitic infections—eosinophils rush in to help defend you. They release chemicals that fight off invaders, but this same response can also cause allergy symptoms such as sneezing, wheezing, or skin rashes.
In normal amounts, eosinophils are important for keeping your body safe. However, when levels are too high or too low, it can point to underlying health conditions. High eosinophil counts often suggest allergies, asthma, or a parasitic infection, while very low levels may affect how well your immune system responds.
Understanding what eosinophils do helps explain why testing them is useful for spotting hidden issues with your immune system and overall health.
Eosinophils are more than just allergy-fighters — they play a subtle but powerful role in maintaining your long-term health, metabolic balance, and resilience against chronic inflammation.
Elevated eosinophil levels are strongly associated with allergic conditions, asthma, and chronic airway inflammation. In Australia, asthma affects about 10% of the population, and blood eosinophilia is often a key biomarker in identifying the “eosinophilic asthma” subtype.
Managing eosinophil-driven inflammation helps reduce flare-ups, tissue damage, and the burden of long-term respiratory disease.
Recent research shows eosinophils help regulate metabolic homeostasis in fat tissue, influencing glucose use, inflammation in visceral fat, and oxidative stress. In animal models, boosting eosinophil activity improved metabolic markers even in high-fat diets, suggesting they help prevent metabolic dysfunctions like insulin resistance.
Over time, keeping inflammation in check and metabolic pathways running smoothly may support healthier ageing and reduce chronic disease burden.
Because eosinophils sit at the crossroads of immunity, inflammation and metabolism, knowing your eosinophil count gives insight not only into allergy or parasite risk but into your body’s deeper balance and resilience.
You may not always notice changes in your eosinophil levels, but certain situations make testing especially important. Consider asking your GP about an eosinophils blood test if you have:
Testing eosinophils in the right context provides a clearer picture of your immune response and can help guide appropriate treatment or preventive steps.
An eosinophils test is typically part of a full blood count or differential white cell count, taken from a small blood sample drawn from your arm in a pathology collection centre.
You do not need to fast for an eosinophils test. You can eat and drink normally, unless other tests (e.g. glucose or lipid panels) are also ordered that require fasting.
Medicare covers many pathology tests through the Medicare Benefits Scheme (MBS), provided certain conditions are met (e.g. requested by a registered practitioner, done in an accredited pathology lab).
But not all tests or variations qualify—some tests may not have a Medicare rebate or may require eligibility criteria. Private pathology providers may charge a fee above the Medicare rebate (“gap”), or may fully bill you if the test isn’t MBS-listed.
For example, Dorevitch Pathology states they may charge more than the rebate if you are non-concessional or if tests aren’t MBS eligible. Some providers cap out-of-pocket costs (e.g. $320 per outpatient visit) for tests eligible under MBS.
Eosinophils count is often included in broader blood count panels or immune / inflammation panels. You don’t always order it standalone; rather it’s bundled with a full blood count (FBC) or white cell differential panel. Your GP can request such a comprehensive panel, which increases the value of the test by giving context across multiple immune cells.
An eosinophils test shows how many of these white blood cells are present in your blood. Results are given in x10⁹/L. Most adults have a count below 0.7 x10⁹/L, but values outside this range can provide important clues about your health.
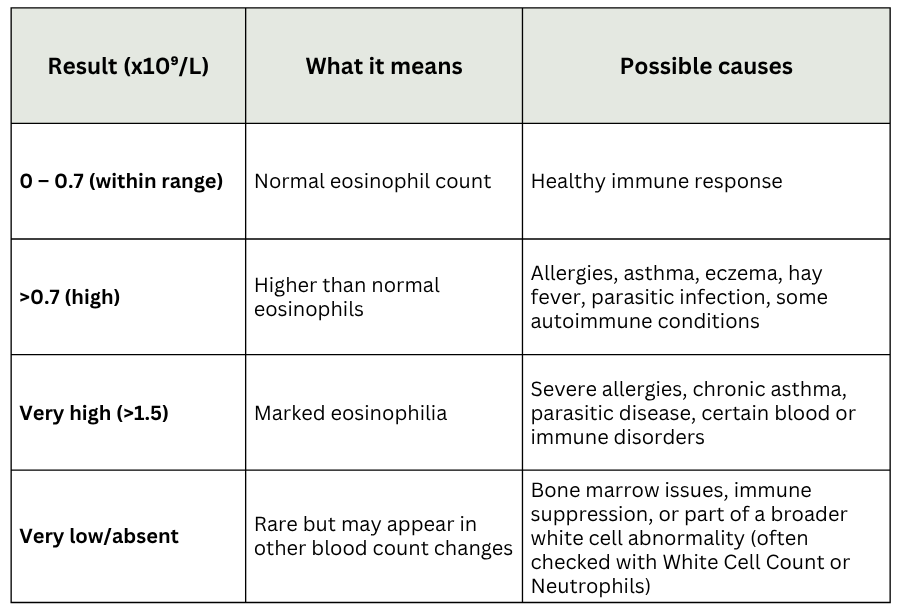
Understanding eosinophil levels is easier when viewed alongside other markers like White Blood Cell Count, Neutrophils, or C-Reactive Protein, as they help identify whether inflammation, infection, or an allergic response is driving the result.
Always discuss your results with your GP or specialist to put them in the right context for your health.
Eosinophil counts give useful information, but they don’t tell the whole story on their own. Doctors usually interpret them as part of a full blood count (FBC) and other immune or inflammation markers to see the bigger picture. For example, high eosinophils with normal white cells may point to allergies, while high eosinophils with raised inflammatory markers could suggest something more systemic.
Related tests that are often considered include:
By looking at eosinophils alongside these markers, your GP or specialist can better understand whether your results reflect a short-term issue, a chronic allergy, or something requiring further investigation. This connected approach ensures you get a more accurate view of your immune and overall health.
While eosinophil levels are mainly influenced by allergies, asthma, infections, and immune responses, certain lifestyle and nutrition choices can support a healthier balance. These approaches are not medical treatments but can help reduce triggers that often drive higher counts.
The best starting point is testing — once you know your levels, you can take personalised steps.
If ordered by your GP for a medical reason, the test is usually covered by Medicare. Without a referral, private costs may range from $30–$60, depending on the provider.
Yes, Medicare covers the eosinophils test when requested by a doctor and performed through an accredited pathology lab. Private requests without referral are not rebated.
In most cases, yes. Your GP or specialist will order the test as part of a full blood count to investigate allergies, asthma, or other conditions.
Yes, it is safe during pregnancy. Doctors may request it if you have asthma, persistent allergies, or unexplained symptoms.
Ongoing wheezing, chronic hay fever, eczema, skin rashes, unexplained digestive issues, or suspected parasitic infections may prompt testing.
The typical reference range is 0–0.7 x10⁹/L. Higher values may suggest allergies, asthma, or parasitic infections.
No, fasting is not needed for an eosinophils test. You can eat and drink normally unless other tests are ordered at the same time.
Eosinophils are specialised white blood cells that protect the body from parasites and play a major role in allergic responses such as asthma, hay fever, and eczema. While they are essential for immune defence, unusually high or low levels can point to hidden issues ranging from allergies and infections to more complex immune conditions. Because these cells sit at the intersection of immunity, inflammation, and overall wellbeing, monitoring their levels can provide valuable clues about your health.
Getting an eosinophils test is a simple, reliable way to better understand what may be driving ongoing symptoms like wheezing, rashes, or digestive discomfort. More importantly, knowing your results empowers you to make informed decisions with your doctor, helping you prevent complications and manage conditions more effectively.
Curious about what your eosinophil count means? Get a Full Body Health Check and explore a complete breakdown of more than 80 key markers.
Subscribe to our newsletter & join a community of 20,000+ Aussies

An eosinophils blood test measures the number of eosinophils, a type of white blood cell that helps fight parasites and is active in allergic conditions like hay fever, asthma, and other immune reactions.
Elevated eosinophil levels are often linked to allergies or parasitic infections. While not directly tied to weight, ongoing allergic inflammation or parasitic illness can affect digestion, energy, and overall wellbeing. Understanding your eosinophil count provides important insight into immune function and potential underlying health issues.
This guide explains what it is, how it works, what your results mean, and how you can book a comprehensive blood test to check your eosinophils.
Eosinophils are a type of white blood cell that play a key role in your immune system. Think of them as your body’s “allergy and parasite fighters.” When the body detects certain triggers—like pollen, dust, or parasitic infections—eosinophils rush in to help defend you. They release chemicals that fight off invaders, but this same response can also cause allergy symptoms such as sneezing, wheezing, or skin rashes.
In normal amounts, eosinophils are important for keeping your body safe. However, when levels are too high or too low, it can point to underlying health conditions. High eosinophil counts often suggest allergies, asthma, or a parasitic infection, while very low levels may affect how well your immune system responds.
Understanding what eosinophils do helps explain why testing them is useful for spotting hidden issues with your immune system and overall health.
Eosinophils are more than just allergy-fighters — they play a subtle but powerful role in maintaining your long-term health, metabolic balance, and resilience against chronic inflammation.
Elevated eosinophil levels are strongly associated with allergic conditions, asthma, and chronic airway inflammation. In Australia, asthma affects about 10% of the population, and blood eosinophilia is often a key biomarker in identifying the “eosinophilic asthma” subtype.
Managing eosinophil-driven inflammation helps reduce flare-ups, tissue damage, and the burden of long-term respiratory disease.
Recent research shows eosinophils help regulate metabolic homeostasis in fat tissue, influencing glucose use, inflammation in visceral fat, and oxidative stress. In animal models, boosting eosinophil activity improved metabolic markers even in high-fat diets, suggesting they help prevent metabolic dysfunctions like insulin resistance.
Over time, keeping inflammation in check and metabolic pathways running smoothly may support healthier ageing and reduce chronic disease burden.
Because eosinophils sit at the crossroads of immunity, inflammation and metabolism, knowing your eosinophil count gives insight not only into allergy or parasite risk but into your body’s deeper balance and resilience.
You may not always notice changes in your eosinophil levels, but certain situations make testing especially important. Consider asking your GP about an eosinophils blood test if you have:
Testing eosinophils in the right context provides a clearer picture of your immune response and can help guide appropriate treatment or preventive steps.
An eosinophils test is typically part of a full blood count or differential white cell count, taken from a small blood sample drawn from your arm in a pathology collection centre.
You do not need to fast for an eosinophils test. You can eat and drink normally, unless other tests (e.g. glucose or lipid panels) are also ordered that require fasting.
Medicare covers many pathology tests through the Medicare Benefits Scheme (MBS), provided certain conditions are met (e.g. requested by a registered practitioner, done in an accredited pathology lab).
But not all tests or variations qualify—some tests may not have a Medicare rebate or may require eligibility criteria. Private pathology providers may charge a fee above the Medicare rebate (“gap”), or may fully bill you if the test isn’t MBS-listed.
For example, Dorevitch Pathology states they may charge more than the rebate if you are non-concessional or if tests aren’t MBS eligible. Some providers cap out-of-pocket costs (e.g. $320 per outpatient visit) for tests eligible under MBS.
Eosinophils count is often included in broader blood count panels or immune / inflammation panels. You don’t always order it standalone; rather it’s bundled with a full blood count (FBC) or white cell differential panel. Your GP can request such a comprehensive panel, which increases the value of the test by giving context across multiple immune cells.
An eosinophils test shows how many of these white blood cells are present in your blood. Results are given in x10⁹/L. Most adults have a count below 0.7 x10⁹/L, but values outside this range can provide important clues about your health.
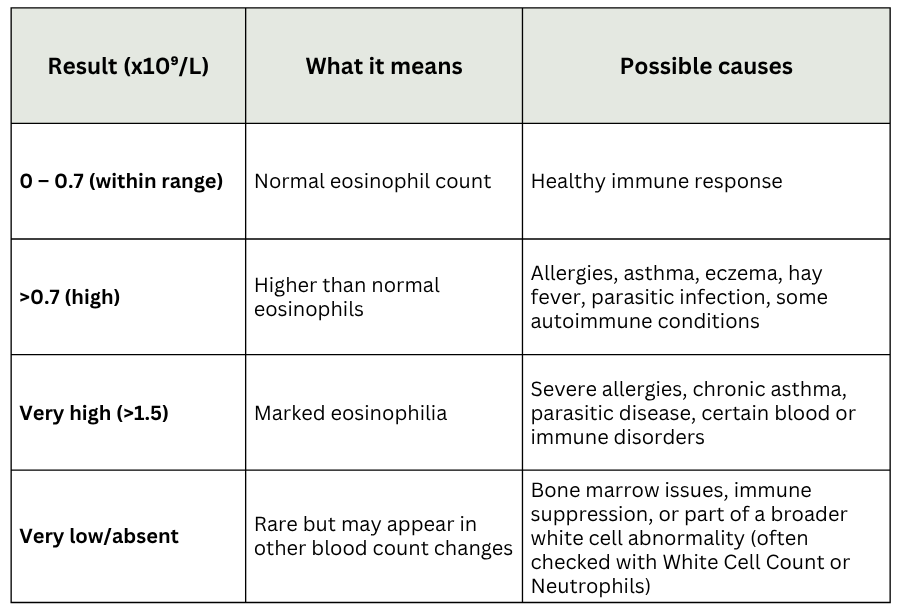
Understanding eosinophil levels is easier when viewed alongside other markers like White Blood Cell Count, Neutrophils, or C-Reactive Protein, as they help identify whether inflammation, infection, or an allergic response is driving the result.
Always discuss your results with your GP or specialist to put them in the right context for your health.
Eosinophil counts give useful information, but they don’t tell the whole story on their own. Doctors usually interpret them as part of a full blood count (FBC) and other immune or inflammation markers to see the bigger picture. For example, high eosinophils with normal white cells may point to allergies, while high eosinophils with raised inflammatory markers could suggest something more systemic.
Related tests that are often considered include:
By looking at eosinophils alongside these markers, your GP or specialist can better understand whether your results reflect a short-term issue, a chronic allergy, or something requiring further investigation. This connected approach ensures you get a more accurate view of your immune and overall health.
While eosinophil levels are mainly influenced by allergies, asthma, infections, and immune responses, certain lifestyle and nutrition choices can support a healthier balance. These approaches are not medical treatments but can help reduce triggers that often drive higher counts.
The best starting point is testing — once you know your levels, you can take personalised steps.
If ordered by your GP for a medical reason, the test is usually covered by Medicare. Without a referral, private costs may range from $30–$60, depending on the provider.
Yes, Medicare covers the eosinophils test when requested by a doctor and performed through an accredited pathology lab. Private requests without referral are not rebated.
In most cases, yes. Your GP or specialist will order the test as part of a full blood count to investigate allergies, asthma, or other conditions.
Yes, it is safe during pregnancy. Doctors may request it if you have asthma, persistent allergies, or unexplained symptoms.
Ongoing wheezing, chronic hay fever, eczema, skin rashes, unexplained digestive issues, or suspected parasitic infections may prompt testing.
The typical reference range is 0–0.7 x10⁹/L. Higher values may suggest allergies, asthma, or parasitic infections.
No, fasting is not needed for an eosinophils test. You can eat and drink normally unless other tests are ordered at the same time.
Eosinophils are specialised white blood cells that protect the body from parasites and play a major role in allergic responses such as asthma, hay fever, and eczema. While they are essential for immune defence, unusually high or low levels can point to hidden issues ranging from allergies and infections to more complex immune conditions. Because these cells sit at the intersection of immunity, inflammation, and overall wellbeing, monitoring their levels can provide valuable clues about your health.
Getting an eosinophils test is a simple, reliable way to better understand what may be driving ongoing symptoms like wheezing, rashes, or digestive discomfort. More importantly, knowing your results empowers you to make informed decisions with your doctor, helping you prevent complications and manage conditions more effectively.
Curious about what your eosinophil count means? Get a Full Body Health Check and explore a complete breakdown of more than 80 key markers.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
