Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan



Weight loss medications may assist in managing obesity when lifestyle changes alone have not led to sufficient results. These options are prescribed under the supervision of a registered healthcare professional, based on individual medical assessments.
Here's a quick overview:
Quick comparison

Note: Side effects like nausea or digestive issues are common but often temporary. Always consult a doctor to find the right medication for your needs and combine it with a healthy diet and exercise for long-term success.
If considering weight loss medication, it helps to understand the factors influencing your weight. Vively’s Weight Management Test looks at key markers linked to insulin resistance, metabolic health, and hormones involved in weight regulation.
Weight loss medications work in various ways to help manage weight effectively. Understanding these mechanisms can help set realistic expectations.
GLP-1 receptor agonists play a key role in weight management. These drugs work by slowing down how quickly the stomach empties and reducing hunger signals in the brain, particularly in the hypothalamus.
Clinical trials have shown that semaglutide, when prescribed and monitored appropriately, may support significant weight loss. In one phase III study, participants on semaglutide 2.4 mg reported an average weight loss of 16.0% compared to 5.7% for the placebo group.
While GLP-1 medications show promise, traditional options also offer alternative approaches to weight loss.
Want to improve your long-term health? Learn why metabolic fitness is important and how it supports better energy, weight balance, and overall wellbeing.
Traditional weight loss medications use different mechanisms to aid in weight reduction:

Phentermine is believed to reduce appetite, and orlistat may reduce fat absorption by inhibiting digestive enzymes. These effects have been observed in clinical studies and vary per individual.
For some individuals, combination therapies offer a more comprehensive approach by targeting multiple pathways. These treatments often pair standard medications with GLP-1 agents to improve weight loss outcomes. For example, bupropion/naltrexone has been studied for its effect on appetite control via the melanocortin system. However, treatment response varies and must be assessed by a doctor.

While multi-drug treatments can be effective, evidence supporting their combined use remains limited. Each approach should be tailored to individual needs and medical guidance.
These medications are usually prescribed to adults with a BMI over 30 or over 27 with related health conditions. A doctor will assess your eligibility.
Eligibility for these medications depends on specific health criteria, with a primary focus on body mass index (BMI). Here’s how the thresholds break down:

For individuals with a BMI over 27, qualifying weight-related conditions include:
According to data from My Weight Loss Clinic, patients with both Type 2 Diabetes and high blood pressure experienced an average weight loss of 8% within the first three months of starting medication therapy in 2024.
Once eligibility is confirmed, treatment begins under the structured guidance of a healthcare provider.
If you're comparing your options, explore our complete guide to Ozempic in Australia for a closer look at how it stacks up against other medications.
After determining eligibility, medical supervision ensures treatments are both safe and effective.
The process starts with a thorough evaluation by a healthcare provider, which includes:
Prescriptions for weight loss medications in Australia must be issued by a practitioner registered with the Australian Health Practitioner Regulation Agency (AHPRA).
Before prescribing medications like GLP-1 agonists (e.g., Wegovy or Saxenda), doctors may require patients to try alternative treatments, such as Metformin, for a set period.
You can also read our complete guide to Mounjaro in Australia to understand how it supports blood sugar control and long-term weight loss.
Weight loss medications are generally used alongside a balanced diet and regular exercise, under medical guidance. This combined approach has been shown in studies to support long-term weight management in eligible individuals.
To get the most out of weight loss medications, it's important to pair them with well-structured eating plans. The type of diet you follow can even influence when you start using these medications. For example, ketogenic diets might delay the need for medication since ketones naturally help curb appetite.
Incorporating these dietary changes with regular physical activity can amplify your progress and overall health benefits.
Exercise plays a key role alongside weight loss medications. It helps by increasing your metabolism, building lean muscle, improving how your body handles insulin, and aiding in long-term weight management.
Here’s a suggested weekly activity breakdown:
Start at a pace that feels manageable and gradually increase intensity as your fitness improves. Collaborate with your healthcare provider to create a plan that aligns with your fitness level and any specific health needs.
Keep in mind, lasting weight loss is about balance - medications are there to support your efforts in diet and exercise, not to replace them.
Looking for simple tools to boost your progress? Our blog on Weighted vests: the best weight loss hack explores how small changes can make a big metabolic impact.
All medicines carry risks. The TGA requires that medications only be advertised for their approved uses, and patients should be aware that individual responses vary. Speak with your doctor or pharmacist before starting any treatment.
Different weight loss medications come with their own set of side effects, with digestive issues being particularly common in GLP-1 receptor agonists.

In most cases, these side effects lessen over time as your body adjusts to the medication. For example, digestive symptoms often improve within a few weeks.
Close monitoring is essential to ensure the medication is both effective and safe.
Medical oversight:
Warning signs to watch for:
The FDA has also updated warnings for medications like Ozempic to include the risk of ileus (a blockage in the intestines). Additionally, if you don’t lose at least 3–4% of your body weight within 12–16 weeks, your doctor may recommend discontinuing the treatment.
Costs vary widely depending on the medication and PBS eligibility. Some treatments are subsidised for diabetes, but obesity-specific options often aren't covered.
The cost of weight loss medications can vary widely, largely influenced by whether they are subsidised under the Pharmaceutical Benefits Scheme (PBS). The availability of PBS subsidies depends on the medicine's approved indication.
For example, Ozempic is subsidised only for type 2 diabetes and not for weight loss. Using medicines off-label may result in higher out-of-pocket costs and should be discussed with a qualified health professional.

Clinical trials reveal that tirzepatide can reduce body fat by 25% within the first year, compared to a 15% reduction for semaglutide.
This stark difference in costs highlights the urgent need for diverse and accessible payment solutions.
The PBS currently limits subsidies for obesity treatments, leaving many patients to bear the full cost.
Government support programs:
The Pharmaceutical Benefits Advisory Committee (PBAC) estimates that subsidising semaglutide for obesity would cost over $1 billion annually over a six-year period.
Private insurers are also reevaluating their coverage policies due to ongoing supply shortages and increased off-label use of these medications.
Financial options:
For diabetes patients, PBS subsidies make these treatments far more affordable. However, the disparity in costs for obesity-specific medications underscores the pressing need for more equitable access to these therapies. Addressing this gap is essential for broader, fairer healthcare solutions.
Now that you've assessed your eligibility and had an initial consultation, it's time to focus on the actionable steps for effective weight management.
Start by organising your health records and setting clear weight loss goals to discuss with your healthcare provider. Being prepared ensures you make the most of your consultation.
"Weight loss medications can be helpful, but they work best when paired with the right habits. Real progress comes from understanding your body and supporting it with consistent, sustainable choices." – Charlotte Battle, APD and Vively’s lead dietitian
Gather the following:
Having this information ready helps streamline the conversation and allows you to ask specific, focused questions during your appointment.

Work with your healthcare team to finalise:
Also, consult your pharmacist about proper medication storage, timing, and any potential interactions with other medications or supplements.
Stay in close contact with your healthcare team to ensure steady progress. Pairing your prescription plan with mindful eating and regular physical activity is essential for long-term success.
Weight loss medications can sometimes bring along side effects, which may differ depending on the specific drug. Common issues include nausea, vomiting, diarrhoea, constipation, and stomach discomfort. Other potential side effects might involve headaches, dizziness, fatigue, insomnia, and shifts in appetite. In certain cases, these medications could also lead to an increased heart rate or blood pressure.
To help minimise these effects, starting with a low dose and gradually increasing it under your healthcare provider's guidance can make a difference. Simple steps like staying hydrated, eating small, balanced meals, and engaging in light physical activity may also provide relief. If the side effects persist or worsen, it’s important to reach out to your doctor. They can adjust your treatment or offer advice that aligns with your specific needs.
The price of weight loss medications in Australia can differ significantly based on the specific drug and its purpose. For instance, tirzepatide (Mounjaro) typically costs between $345 and $645 per month, while semaglutide (Ozempic) is priced at around $42 per month under the Pharmaceutical Benefits Scheme (PBS) for managing type 2 diabetes. However, if prescribed off-label for obesity, the cost rises to about $133 per month. Another option, Wegovy, which also contains semaglutide, is available but tends to be on the pricier side.
To make these treatments more accessible, some manufacturers provide patient support programs that can lower expenses for those who qualify. If you're thinking about starting these medications, it's a good idea to talk to your healthcare provider or pharmacist about costs and any available financial assistance programs.
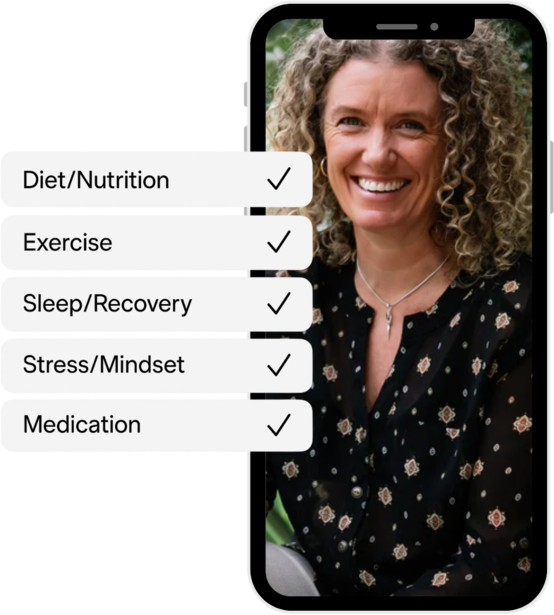
When using weight loss medications, pairing them with healthy lifestyle choices is key to getting the best results. These medications work hand-in-hand with your body’s natural systems, but their impact is significantly greater when combined with proper diet and regular exercise.
Staying active through consistent physical activity helps burn fat, preserve muscle, and boost overall health. At the same time, a well-rounded diet supports the medication’s role while building habits that can stick for the long haul. Together, these efforts not only amplify the medication’s benefits but also set the stage for maintaining your progress long after the treatment concludes.
Important disclaimer: This guide is intended for general informational purposes only and does not substitute professional medical advice. All prescription weight loss medications should be taken only under the supervision of a registered medical practitioner. Claims about medication efficacy are based on clinical studies and may not apply to all individuals.
This content aligns with the Therapeutic Goods Administration (TGA) and Australian Health Practitioner Regulation Agency (AHPRA) guidelines as of publication. For personalised advice, consult your GP or healthcare provider.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Weight loss medications may assist in managing obesity when lifestyle changes alone have not led to sufficient results. These options are prescribed under the supervision of a registered healthcare professional, based on individual medical assessments.
Here's a quick overview:
Quick comparison

Note: Side effects like nausea or digestive issues are common but often temporary. Always consult a doctor to find the right medication for your needs and combine it with a healthy diet and exercise for long-term success.
If considering weight loss medication, it helps to understand the factors influencing your weight. Vively’s Weight Management Test looks at key markers linked to insulin resistance, metabolic health, and hormones involved in weight regulation.
Weight loss medications work in various ways to help manage weight effectively. Understanding these mechanisms can help set realistic expectations.
GLP-1 receptor agonists play a key role in weight management. These drugs work by slowing down how quickly the stomach empties and reducing hunger signals in the brain, particularly in the hypothalamus.
Clinical trials have shown that semaglutide, when prescribed and monitored appropriately, may support significant weight loss. In one phase III study, participants on semaglutide 2.4 mg reported an average weight loss of 16.0% compared to 5.7% for the placebo group.
While GLP-1 medications show promise, traditional options also offer alternative approaches to weight loss.
Want to improve your long-term health? Learn why metabolic fitness is important and how it supports better energy, weight balance, and overall wellbeing.
Traditional weight loss medications use different mechanisms to aid in weight reduction:

Phentermine is believed to reduce appetite, and orlistat may reduce fat absorption by inhibiting digestive enzymes. These effects have been observed in clinical studies and vary per individual.
For some individuals, combination therapies offer a more comprehensive approach by targeting multiple pathways. These treatments often pair standard medications with GLP-1 agents to improve weight loss outcomes. For example, bupropion/naltrexone has been studied for its effect on appetite control via the melanocortin system. However, treatment response varies and must be assessed by a doctor.

While multi-drug treatments can be effective, evidence supporting their combined use remains limited. Each approach should be tailored to individual needs and medical guidance.
These medications are usually prescribed to adults with a BMI over 30 or over 27 with related health conditions. A doctor will assess your eligibility.
Eligibility for these medications depends on specific health criteria, with a primary focus on body mass index (BMI). Here’s how the thresholds break down:

For individuals with a BMI over 27, qualifying weight-related conditions include:
According to data from My Weight Loss Clinic, patients with both Type 2 Diabetes and high blood pressure experienced an average weight loss of 8% within the first three months of starting medication therapy in 2024.
Once eligibility is confirmed, treatment begins under the structured guidance of a healthcare provider.
If you're comparing your options, explore our complete guide to Ozempic in Australia for a closer look at how it stacks up against other medications.
After determining eligibility, medical supervision ensures treatments are both safe and effective.
The process starts with a thorough evaluation by a healthcare provider, which includes:
Prescriptions for weight loss medications in Australia must be issued by a practitioner registered with the Australian Health Practitioner Regulation Agency (AHPRA).
Before prescribing medications like GLP-1 agonists (e.g., Wegovy or Saxenda), doctors may require patients to try alternative treatments, such as Metformin, for a set period.
You can also read our complete guide to Mounjaro in Australia to understand how it supports blood sugar control and long-term weight loss.
Weight loss medications are generally used alongside a balanced diet and regular exercise, under medical guidance. This combined approach has been shown in studies to support long-term weight management in eligible individuals.
To get the most out of weight loss medications, it's important to pair them with well-structured eating plans. The type of diet you follow can even influence when you start using these medications. For example, ketogenic diets might delay the need for medication since ketones naturally help curb appetite.
Incorporating these dietary changes with regular physical activity can amplify your progress and overall health benefits.
Exercise plays a key role alongside weight loss medications. It helps by increasing your metabolism, building lean muscle, improving how your body handles insulin, and aiding in long-term weight management.
Here’s a suggested weekly activity breakdown:
Start at a pace that feels manageable and gradually increase intensity as your fitness improves. Collaborate with your healthcare provider to create a plan that aligns with your fitness level and any specific health needs.
Keep in mind, lasting weight loss is about balance - medications are there to support your efforts in diet and exercise, not to replace them.
Looking for simple tools to boost your progress? Our blog on Weighted vests: the best weight loss hack explores how small changes can make a big metabolic impact.
All medicines carry risks. The TGA requires that medications only be advertised for their approved uses, and patients should be aware that individual responses vary. Speak with your doctor or pharmacist before starting any treatment.
Different weight loss medications come with their own set of side effects, with digestive issues being particularly common in GLP-1 receptor agonists.

In most cases, these side effects lessen over time as your body adjusts to the medication. For example, digestive symptoms often improve within a few weeks.
Close monitoring is essential to ensure the medication is both effective and safe.
Medical oversight:
Warning signs to watch for:
The FDA has also updated warnings for medications like Ozempic to include the risk of ileus (a blockage in the intestines). Additionally, if you don’t lose at least 3–4% of your body weight within 12–16 weeks, your doctor may recommend discontinuing the treatment.
Costs vary widely depending on the medication and PBS eligibility. Some treatments are subsidised for diabetes, but obesity-specific options often aren't covered.
The cost of weight loss medications can vary widely, largely influenced by whether they are subsidised under the Pharmaceutical Benefits Scheme (PBS). The availability of PBS subsidies depends on the medicine's approved indication.
For example, Ozempic is subsidised only for type 2 diabetes and not for weight loss. Using medicines off-label may result in higher out-of-pocket costs and should be discussed with a qualified health professional.

Clinical trials reveal that tirzepatide can reduce body fat by 25% within the first year, compared to a 15% reduction for semaglutide.
This stark difference in costs highlights the urgent need for diverse and accessible payment solutions.
The PBS currently limits subsidies for obesity treatments, leaving many patients to bear the full cost.
Government support programs:
The Pharmaceutical Benefits Advisory Committee (PBAC) estimates that subsidising semaglutide for obesity would cost over $1 billion annually over a six-year period.
Private insurers are also reevaluating their coverage policies due to ongoing supply shortages and increased off-label use of these medications.
Financial options:
For diabetes patients, PBS subsidies make these treatments far more affordable. However, the disparity in costs for obesity-specific medications underscores the pressing need for more equitable access to these therapies. Addressing this gap is essential for broader, fairer healthcare solutions.
Now that you've assessed your eligibility and had an initial consultation, it's time to focus on the actionable steps for effective weight management.
Start by organising your health records and setting clear weight loss goals to discuss with your healthcare provider. Being prepared ensures you make the most of your consultation.
"Weight loss medications can be helpful, but they work best when paired with the right habits. Real progress comes from understanding your body and supporting it with consistent, sustainable choices." – Charlotte Battle, APD and Vively’s lead dietitian
Gather the following:
Having this information ready helps streamline the conversation and allows you to ask specific, focused questions during your appointment.

Work with your healthcare team to finalise:
Also, consult your pharmacist about proper medication storage, timing, and any potential interactions with other medications or supplements.
Stay in close contact with your healthcare team to ensure steady progress. Pairing your prescription plan with mindful eating and regular physical activity is essential for long-term success.
Weight loss medications can sometimes bring along side effects, which may differ depending on the specific drug. Common issues include nausea, vomiting, diarrhoea, constipation, and stomach discomfort. Other potential side effects might involve headaches, dizziness, fatigue, insomnia, and shifts in appetite. In certain cases, these medications could also lead to an increased heart rate or blood pressure.
To help minimise these effects, starting with a low dose and gradually increasing it under your healthcare provider's guidance can make a difference. Simple steps like staying hydrated, eating small, balanced meals, and engaging in light physical activity may also provide relief. If the side effects persist or worsen, it’s important to reach out to your doctor. They can adjust your treatment or offer advice that aligns with your specific needs.
The price of weight loss medications in Australia can differ significantly based on the specific drug and its purpose. For instance, tirzepatide (Mounjaro) typically costs between $345 and $645 per month, while semaglutide (Ozempic) is priced at around $42 per month under the Pharmaceutical Benefits Scheme (PBS) for managing type 2 diabetes. However, if prescribed off-label for obesity, the cost rises to about $133 per month. Another option, Wegovy, which also contains semaglutide, is available but tends to be on the pricier side.
To make these treatments more accessible, some manufacturers provide patient support programs that can lower expenses for those who qualify. If you're thinking about starting these medications, it's a good idea to talk to your healthcare provider or pharmacist about costs and any available financial assistance programs.
When using weight loss medications, pairing them with healthy lifestyle choices is key to getting the best results. These medications work hand-in-hand with your body’s natural systems, but their impact is significantly greater when combined with proper diet and regular exercise.
Staying active through consistent physical activity helps burn fat, preserve muscle, and boost overall health. At the same time, a well-rounded diet supports the medication’s role while building habits that can stick for the long haul. Together, these efforts not only amplify the medication’s benefits but also set the stage for maintaining your progress long after the treatment concludes.
Important disclaimer: This guide is intended for general informational purposes only and does not substitute professional medical advice. All prescription weight loss medications should be taken only under the supervision of a registered medical practitioner. Claims about medication efficacy are based on clinical studies and may not apply to all individuals.
This content aligns with the Therapeutic Goods Administration (TGA) and Australian Health Practitioner Regulation Agency (AHPRA) guidelines as of publication. For personalised advice, consult your GP or healthcare provider.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
