Choose how you’d like to begin
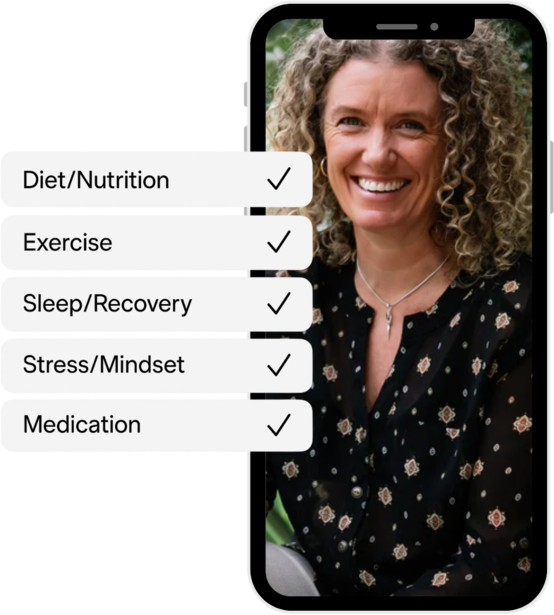
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan



Can COVID cause insomnia? This article explores the causes, symptoms, and treatment of post-COVID insomnia. Discover how stress, weakened immune response, and persistent COVID-19 symptoms can contribute to sleep deprivation. Learn how to prevent or reduce the effects of insomnia and improve your overall sleep quality.
Is insomnia a symptom of COVID? While insomnia is not commonly recognised as a primary symptom of COVID-19, a significant number of post-COVID patients in Australia are experiencing sleep disturbances. This article delves into the causes, symptoms, and potential treatment options for sleep deprivation following a COVID-19 infection.
There are various causes of post-COVID insomnia, and each person may experience it differently.
Stress and anxiety may contribute to post-COVID insomnia. Stress caused by a variety of factors may be associated with insomnia, this includes job loss, loneliness resulting from the COVID-19 lockdown or being in hospital, financial difficulties, and even losing friends and family members to COVID-19 infections.
Some COVID-19 symptoms, such as shortness of breath and chest pain, may also persist during recovery, resulting in a constant lack of sleep.
Insomnia after COVID may also be caused by the body's weakened immune response. It's worth noting that the virus damages not only the lungs but also the nervous system, making it more fragile and prone to inflammation. This impairs the brain's ability to shut down when it should, leading to a reduced quality of sleep and poor mental health outcomes.
Certain medications used during the treatment of the COVID infection can have side effects that disrupt normal sleep patterns. While these medications are necessary for managing the virus and its symptoms, they can inadvertently cause sleep disturbances as an unintended consequence. It is important to consider the potential impact of medications on sleep when addressing post-COVID insomnia.
On average, post-COVID insomnia lasts for about two weeks. However, some people may unfortunately experience sleep issues for longer periods of time.
The prevalence of sleep problems, causing abnormal wake-sleep cycles, is a hallmark of insomnia, regardless of whether it's short-term or chronic insomnia. However, if you've never suffered from any sleep disorders before the COVID-19 outbreak, it may be linked to the illness.
The symptoms of insomnia vary according to the differences in insomnia classifications. Some of these are temporary, while others can last for months, as is the case with severe insomnia. However, the following are the most common symptoms of insomnia:
If not treated properly, post-COVID insomnia can lead to a variety of other issues, including:
If you're experiencing insomnia and any of the above symptoms, it's important to seek professional help from your doctor.
If you're experiencing post-COVID-19 insomnia, there are some steps you can take to mitigate its effects.
We strongly advise you to consult with your doctor about your symptoms and treatment options. You can also seek help from a sleep counsellor or specialist or join a support group.
CBT-I is a highly effective treatment for insomnia and has shown promising results for managing post-COVID insomnia. This therapy focuses on identifying and modifying negative thoughts and behaviours that contribute to sleep disturbances. A trained therapist can help individuals develop healthy sleep habits and relaxation techniques, improving sleep quality and promoting better overall wellbeing.
Practising relaxation techniques can help calm the mind and prepare the body for sleep. Deep breathing exercises, progressive muscle relaxation, and meditation are effective methods to promote relaxation before bedtime. These techniques can reduce anxiety, stress, and racing thoughts, allowing for a more peaceful transition into sleep.
Establishing a consistent sleep-wake schedule helps regulate the body's internal clock and promotes better sleep. It is essential to set a regular bedtime and wake-up time, even on weekends or days off. This consistency reinforces the body's natural sleep-wake cycle, making it easier to fall asleep and wake up feeling refreshed.
Engaging in regular physical exercise can have numerous benefits for sleep and overall health. Physical activity promotes the release of endorphins, reduces anxiety, and helps regulate sleep patterns. It is important to choose activities that suit individual preferences and fitness levels, aiming for at least 30 minutes of moderate-intensity exercise most days of the week. However, it is advisable to avoid exercising too close to bedtime, as it may interfere with sleep in some people.
Stimulants like caffeine can disrupt sleep and exacerbate insomnia symptoms. It is advisable to limit or avoid consuming caffeine-containing beverages and foods, such as coffee, tea, energy drinks, and chocolate, especially in the afternoon and evening. Instead, opt for caffeine-free herbal teas or decaffeinated alternatives to promote better sleep quality.
While alcohol may initially induce drowsiness, it can negatively impact sleep quality and exacerbate insomnia symptoms. It is recommended to limit alcohol consumption, especially in the evening, as it can disrupt the natural sleep cycle and lead to fragmented and restless sleep.
Creating a relaxing nighttime routine can signal to the body and mind that it's time to unwind and prepare for sleep. This routine can include activities such as taking a warm bath, reading a book, listening to calming music, drinking a sleep tea or practising relaxation exercises. Consistently following a soothing routine before bed can help promote better sleep onset and improve overall sleep quality.
It is important to consult with a healthcare professional or sleep specialist for personalised guidance and support if you are having trouble sleeping. They can provide individualised recommendations and develop a comprehensive treatment plan tailored to specific needs and circumstances.
If you're looking for additional support in improving your sleep and overall health, consider using Vively, a metabolic health app. Vively offers personalised guidance and tools to help individuals optimise their glucose control, which can positively impact sleep quality and overall well being. Check out Vively to learn more about how their app can assist you in achieving better sleep and overall metabolic health.
In conclusion, post-COVID insomnia is a prevalent issue among individuals who have recovered from COVID-19. Stress, weakened immune response, and persistent COVID-19 symptoms contribute to sleep deprivation. It's important to recognise the symptoms of COVID-related insomnia and seek appropriate treatment to prevent the development of other health problems. By practising healthy sleep habits and seeking professional guidance, individuals can improve their sleep quality and overall well being.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Can COVID cause insomnia? This article explores the causes, symptoms, and treatment of post-COVID insomnia. Discover how stress, weakened immune response, and persistent COVID-19 symptoms can contribute to sleep deprivation. Learn how to prevent or reduce the effects of insomnia and improve your overall sleep quality.
Is insomnia a symptom of COVID? While insomnia is not commonly recognised as a primary symptom of COVID-19, a significant number of post-COVID patients in Australia are experiencing sleep disturbances. This article delves into the causes, symptoms, and potential treatment options for sleep deprivation following a COVID-19 infection.
There are various causes of post-COVID insomnia, and each person may experience it differently.
Stress and anxiety may contribute to post-COVID insomnia. Stress caused by a variety of factors may be associated with insomnia, this includes job loss, loneliness resulting from the COVID-19 lockdown or being in hospital, financial difficulties, and even losing friends and family members to COVID-19 infections.
Some COVID-19 symptoms, such as shortness of breath and chest pain, may also persist during recovery, resulting in a constant lack of sleep.
Insomnia after COVID may also be caused by the body's weakened immune response. It's worth noting that the virus damages not only the lungs but also the nervous system, making it more fragile and prone to inflammation. This impairs the brain's ability to shut down when it should, leading to a reduced quality of sleep and poor mental health outcomes.
Certain medications used during the treatment of the COVID infection can have side effects that disrupt normal sleep patterns. While these medications are necessary for managing the virus and its symptoms, they can inadvertently cause sleep disturbances as an unintended consequence. It is important to consider the potential impact of medications on sleep when addressing post-COVID insomnia.
On average, post-COVID insomnia lasts for about two weeks. However, some people may unfortunately experience sleep issues for longer periods of time.
The prevalence of sleep problems, causing abnormal wake-sleep cycles, is a hallmark of insomnia, regardless of whether it's short-term or chronic insomnia. However, if you've never suffered from any sleep disorders before the COVID-19 outbreak, it may be linked to the illness.
The symptoms of insomnia vary according to the differences in insomnia classifications. Some of these are temporary, while others can last for months, as is the case with severe insomnia. However, the following are the most common symptoms of insomnia:
If not treated properly, post-COVID insomnia can lead to a variety of other issues, including:
If you're experiencing insomnia and any of the above symptoms, it's important to seek professional help from your doctor.
If you're experiencing post-COVID-19 insomnia, there are some steps you can take to mitigate its effects.
We strongly advise you to consult with your doctor about your symptoms and treatment options. You can also seek help from a sleep counsellor or specialist or join a support group.
CBT-I is a highly effective treatment for insomnia and has shown promising results for managing post-COVID insomnia. This therapy focuses on identifying and modifying negative thoughts and behaviours that contribute to sleep disturbances. A trained therapist can help individuals develop healthy sleep habits and relaxation techniques, improving sleep quality and promoting better overall wellbeing.
Practising relaxation techniques can help calm the mind and prepare the body for sleep. Deep breathing exercises, progressive muscle relaxation, and meditation are effective methods to promote relaxation before bedtime. These techniques can reduce anxiety, stress, and racing thoughts, allowing for a more peaceful transition into sleep.
Establishing a consistent sleep-wake schedule helps regulate the body's internal clock and promotes better sleep. It is essential to set a regular bedtime and wake-up time, even on weekends or days off. This consistency reinforces the body's natural sleep-wake cycle, making it easier to fall asleep and wake up feeling refreshed.
Engaging in regular physical exercise can have numerous benefits for sleep and overall health. Physical activity promotes the release of endorphins, reduces anxiety, and helps regulate sleep patterns. It is important to choose activities that suit individual preferences and fitness levels, aiming for at least 30 minutes of moderate-intensity exercise most days of the week. However, it is advisable to avoid exercising too close to bedtime, as it may interfere with sleep in some people.
Stimulants like caffeine can disrupt sleep and exacerbate insomnia symptoms. It is advisable to limit or avoid consuming caffeine-containing beverages and foods, such as coffee, tea, energy drinks, and chocolate, especially in the afternoon and evening. Instead, opt for caffeine-free herbal teas or decaffeinated alternatives to promote better sleep quality.
While alcohol may initially induce drowsiness, it can negatively impact sleep quality and exacerbate insomnia symptoms. It is recommended to limit alcohol consumption, especially in the evening, as it can disrupt the natural sleep cycle and lead to fragmented and restless sleep.
Creating a relaxing nighttime routine can signal to the body and mind that it's time to unwind and prepare for sleep. This routine can include activities such as taking a warm bath, reading a book, listening to calming music, drinking a sleep tea or practising relaxation exercises. Consistently following a soothing routine before bed can help promote better sleep onset and improve overall sleep quality.
It is important to consult with a healthcare professional or sleep specialist for personalised guidance and support if you are having trouble sleeping. They can provide individualised recommendations and develop a comprehensive treatment plan tailored to specific needs and circumstances.
If you're looking for additional support in improving your sleep and overall health, consider using Vively, a metabolic health app. Vively offers personalised guidance and tools to help individuals optimise their glucose control, which can positively impact sleep quality and overall well being. Check out Vively to learn more about how their app can assist you in achieving better sleep and overall metabolic health.
In conclusion, post-COVID insomnia is a prevalent issue among individuals who have recovered from COVID-19. Stress, weakened immune response, and persistent COVID-19 symptoms contribute to sleep deprivation. It's important to recognise the symptoms of COVID-related insomnia and seek appropriate treatment to prevent the development of other health problems. By practising healthy sleep habits and seeking professional guidance, individuals can improve their sleep quality and overall well being.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
