What is bioavailable testosterone?
Bioavailable testosterone is the portion of total testosterone that is not tightly bound to SHBG (sex hormone-binding globulin). It comprises the unbound (free) testosterone plus the fraction loosely bound to albumin. Because it is accessible to tissues (e.g. muscle, fat, brain), it is often considered a better proxy for active androgenic effects than just total testosterone.
Why does it matter for long-term health and wellbeing?
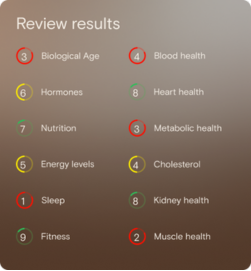
Hormones like testosterone play a modulatory role in energy regulation, body composition, mood, sexual function and metabolic processes. Monitoring bioavailable testosterone gives a more precise insight into the effective hormonal activity your tissues “see.” Over time, small downward shifts outside your optimal zone may signal early drift in metabolic or functional resilience — giving you the chance to act before more noticeable symptoms emerge.
What’s an optimal level of bioavailable testosterone?
Because measurement methods and population baselines vary, there is no universally accepted “textbook” range. Laboratories may report different reference intervals depending on the assay used.
As a guide: in adult men, total testosterone reference ranges in Australian labs often fall around 8–35 nmol/L for younger to middle age, with lower cutoffs around 6–8 nmol/L considered borderline or low in some clinical contexts.
For free or bioavailable testosterone, Australian reference ranges are less commonly published; one Australian pathology handbook lists free testosterone in adult males at ~ 260–740 pmol/L (i.e. 0.26–0.74 nmol/L) per certain assays.
In practical coaching contexts, an “optimal” bioavailable testosterone zone might be set narrower (for instance, mid-to-upper percentiles of a well population), rather than simply the full lab reference interval. (You would confirm with the specific lab’s method.)
What influences bioavailable testosterone levels?
Several key factors can shift bioavailable testosterone, including:
- SHBG concentrations: When SHBG is high, a larger portion of testosterone is bound and unavailable. Liver health, thyroid status, metabolic factors and medications influence SHBG.
- Body composition & adiposity: Higher fat, especially visceral fat, is often associated with lower free/bioavailable testosterone.
- Age: SHBG tends to rise with age, and the free/bioavailable share tends to decline even if total testosterone is preserved.
- Nutrition, sleep, stress, physical activity: These lifestyle factors influence hormonal balance, SHBG expression and testosterone synthesis.
- Medications or supplements: Certain drugs may shift SHBG or testosterone binding dynamics.
What does it mean if bioavailable testosterone is outside the optimal range?
- If your bioavailable level is below your optimal (or lower than the lab’s healthy range), it suggests that even if your total testosterone is “normal,” your tissues may be receiving less androgenic drive. Over time this may translate into reduced energy, muscle loss, metabolic slowing or libido decline (in a wellness framing).
- If your bioavailable level is above optimal, it may suggest that androgenic activity is stronger than needed, potentially correlating with androgen excess symptoms (e.g. skin changes, mood shifts) or overstimulation.
- An out-of-range result is not a diagnosis, but rather a signal worthy of deeper insight, paired with other markers, trend data, and lifestyle context.
How can I support healthy bioavailable testosterone levels?
Here are evidence-aligned lifestyle strategies (non-pharmaceutical) you can use:
- Preserve or build lean muscle through resistance training
- Maintain healthy body composition (reduce excess adiposity)
- Prioritise sleep quality and duration
- Balance macronutrients — sufficient protein, healthy fats, stabilised blood sugar
- Manage long-term stress (chronic cortisol can shift hormonal balance)
- Avoid overtraining or chronic energy deficits
- Support liver health (because SHBG synthesis occurs partly in the liver)
- Check for and optimise micronutrients (e.g. vitamin D, zinc, magnesium) as part of a balanced diet
This information is provided for general health and wellness purposes only and does not replace medical advice.
References
- Yeap, B. B., Grossmann, M., McLachlan, R. I., et al. (2016). Endocrine Society of Australia position statement on male hypogonadism Part 1: Assessment and indications for testosterone therapy. Medical Journal of Australia, 205(4), 173–178.
- Royal College of Pathologists of Australasia. (2024). Testosterone total — RCPA Manual. Retrieved 6 Feb 2024.
- Royal College of Pathologists of Australasia. (2024). SHBG — Sex Hormone Binding Globulin — RCPA Manual. Retrieved 4 Nov 2024.

















.png)


.svg)

