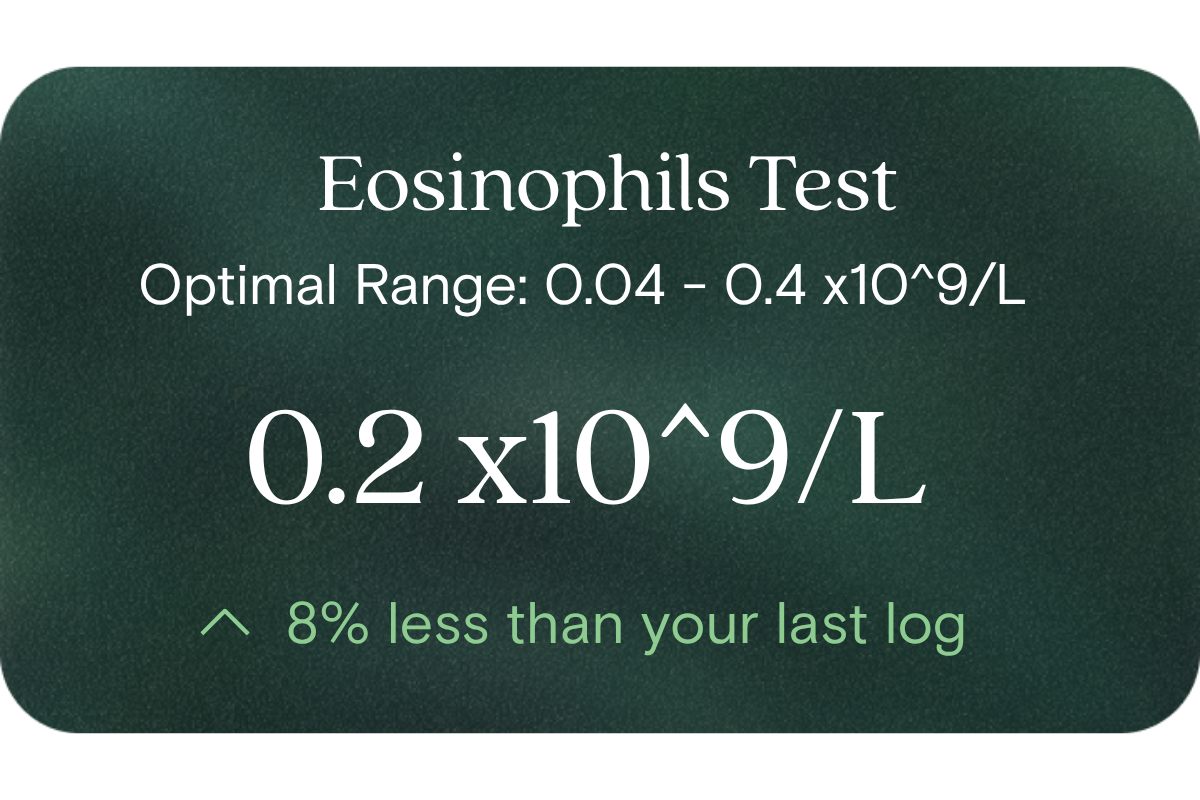
What is Eosinophils?
Eosinophils are a subclass of white blood cells (immune cells) that circulate in your bloodstream and migrate into tissues. Their primary roles involve responding to certain external exposures (for example, parasites, allergens, or environmental triggers). They release mediators that help clear or contain these exposures and contribute to the tissue-level immune balance. They are routinely quantified in a full blood count (FBC) or complete blood count (CBC) test.
Why does it matter for long-term health and wellbeing?
Because eosinophils represent a component of your immune system’s activity, their levels offer a window into your immune load and inflammatory balance. Over time, minor but persistent elevations may reflect continuous exposure or activation (for example by allergens or irritants) that can subtly affect your metabolism, tissue health, and resilience. By contrast, chronically low eosinophil levels might hint that some immune pathways are suppressed, which could reduce robustness against certain challenges. In both cases, tracking changes over time helps you spot trends and adjust lifestyle or environmental factors proactively — supporting vitality and steady immune performance as you age.
What’s an optimal level of Eosinophils?
- Lab (reference) range (Australia): 0.04 to 0.4 ×10⁹/L
- Optimal (target) range: Because there is no universally accepted “optimal” range beyond the lab reference, we recommend aiming to stay comfortably within the middle portion of the reference range (for example, ~0.10 to 0.30 ×10⁹/L) and using your personal baseline and trend lines as your guide.
This ensures you avoid both extremes (too low or too high) while allowing adaptive immune responsiveness. Over time, deviations from your own baseline should trigger a review of possible drivers.
What influences Eosinophils levels?
Many factors modulate eosinophil counts, including:
- Environmental exposures and allergens (pollens, dust mites, moulds, chemicals)
- Parasitic or external microorganism exposures
- Seasonal or geographic changes
- Sleep quality, stress and cortisol rhythms
- Dietary patterns and gut health / microbiome balance
- Circadian rhythms and time of day
- Genetic and individual immune programming
Because of these inputs, day-to-day variability can occur — which is why trends over weeks or months are most informative.
What does it mean if Eosinophils is outside the optimal range?
- Above the upper limit (eosinophilia): This suggests your body may be persistently reacting to some stimulation (for example allergens, environmental triggers, or less common causes). Over time, that could spell a higher baseline immune workload, which may subtly press on metabolic and tissue systems.
- Below the lower limit (eosinopenia): A persistently low count might suggest that some immune pathways are suppressed or underactive relative to your baseline. That could slightly reduce your capacity for certain immune challenges.
In both cases, deviations don’t necessarily imply overt disease; rather, they act as early signals for you to review factors such as exposures, sleep, stress, and gut or environmental health.
How can I support healthy Eosinophils levels?
You can build resilience around eosinophil homeostasis through thoughtful lifestyle and environmental adjustments:
- Reduce allergen and irritant exposures: E.g. air purification, minimise dust, mould remediation, avoid chemical pollutant exposures
- Support gut and microbiome health: Consuming diverse fibre, fermented foods, avoiding excessive processed/ultra-processed foods
- Ensure quality sleep and align with circadian rhythm: Good sleep supports balanced immune regulation
- Manage stress and maintain cortisol balance (e.g. via meditation, movement, breathwork)
- Gradual exposure strategies: In some contexts, controlled exposure (e.g. allergen desensitisation) can help ‘retrain’ immune tolerance
- Monitor and adjust over time: Use your own trend data to guide incremental changes rather than chasing an arbitrary target.
This information is provided for general health and wellness purposes only and does not replace medical advice.
References
- Negewo, N. A., et al. (2016). Peripheral blood eosinophils as a surrogate marker for airway eosinophilia. International Journal of Chronic Obstructive Pulmonary Disease.
- Weaver, M. D. (2024). Review of peripheral blood eosinophilia: workup and mechanisms. MDPI Hematology.
- Pitman, M. C., et al. (2013). Eosinophils in severe sepsis in northern Australia. Critical Care Medicine.
- Corren, J., et al. (2021). Variability in blood eosinophil counts in patients with respiratory disease. Journal of Respiratory Research.
















.png)


.svg)

