What is Fasting Insulin blood test?
Fasting Insulin is the concentration of insulin circulating in your blood after an overnight fast (typically 8–12 hours). It represents the basal output of insulin needed to regulate your blood sugar in a resting state, before dietary glucose begins to influence levels.
Why does it matter for long-term health and wellbeing?
Insulin is central to how your body manages carbohydrates, fat storage, energy use, and hormone signalling. Over time, rising levels seen on a fasting insulin test, even when glucose appears normal, can indicate that tissues such as muscle, liver, and fat are becoming less responsive to insulin.
This shift may reduce metabolic flexibility, increase fat gain, disrupt appetite and hormonal balance, and accelerate pathways that affect longevity and performance. Measuring insulin through a fasting insulin test provides earlier, actionable feedback than waiting for glucose levels to change.
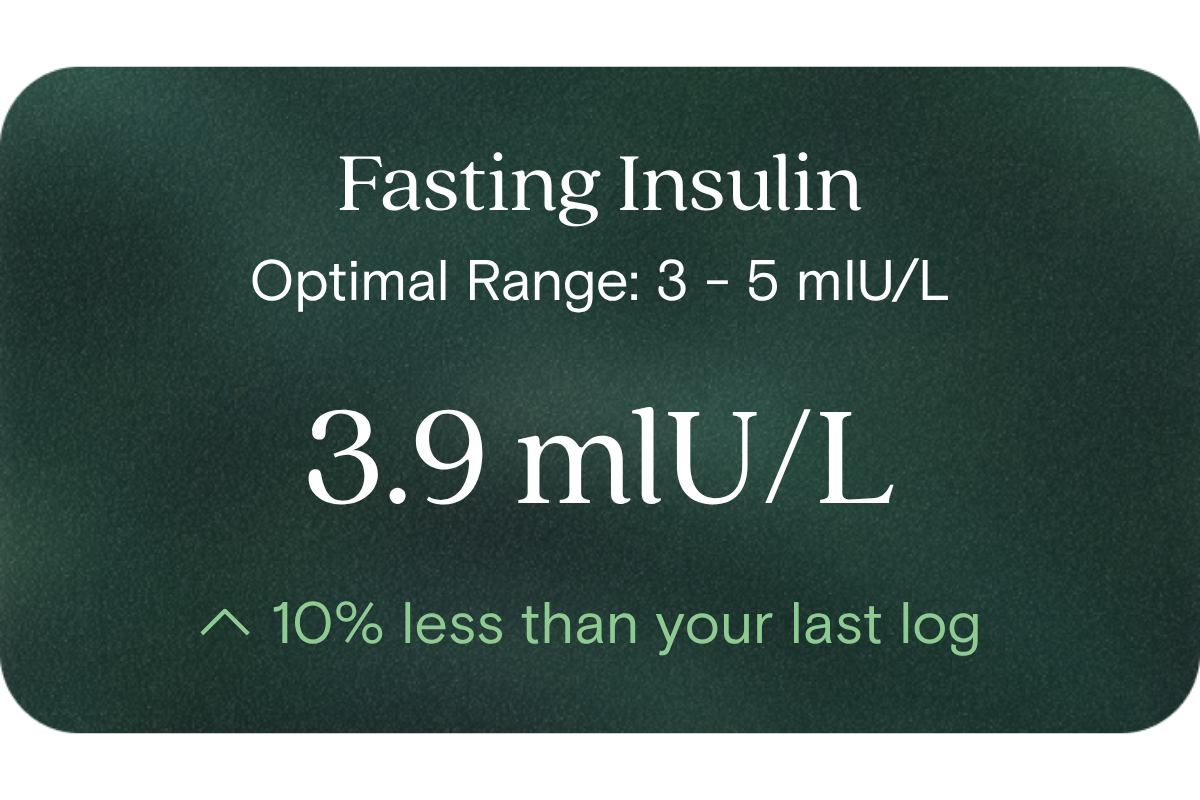
What’s an optimal level of Fasting Insulin?
- Laboratory (reference) range: 3 to 25 mIU/L
- Vively’s optimal target: up to ~7 mIU/L
These values guide where you ideally want to be (under ≈ 7) within the broader “normal” laboratory window of 3–25.
What influences Fasting Insulin levels?
Many modifiable and non-modifiable factors affect fasting insulin, including:
- Diet (especially refined carbs, glycaemic load, meal timing)
- Physical activity, especially resistance and interval training
- Sleep quality and duration
- Stress and cortisol regulation
- Body composition (especially visceral fat)
- Genetic predisposition and ethnicity
- Age
- Insulin secretory dynamics (how aggressively the pancreas responds)
What does it mean if Fasting Insulin is outside the optimal range?
If fasting insulin is above your optimal target, it suggests your body is compensating harder to maintain normal glucose levels. That’s a signal your metabolic system is under strain and may be drifting toward reduced insulin sensitivity. Conversely, values very low (below reference) might reflect under-secretion or other regulatory shifts (though this is much less common in generally healthy people). Either way, values outside your optimal range are not a “diagnosis” — they are insight points indicating opportunity for lifestyle tuning.
How can I support healthy Fasting Insulin levels?
Here are evidence-aligned strategies:
- Emphasise whole, minimally processed foods and moderate your intake of refined carbohydrates
- Introduce strength training / resistance exercise and periodic high-intensity work
- Regular physical activity including non-exercise movement (walking, standing)
- Prioritise consistent, restorative sleep
- Manage stress via mindfulness, breathing practices or recovery routines
- Time your meals mindfully (e.g. avoiding late heavy carbs)
- Monitor other metabolic markers (glucose, lipids, inflammation) to guide your adjustments
This information is provided for general health and wellness purposes only and does not replace medical advice.
References
- Samaras, K., McElduff, A., Twigg, S. M., et al. (2006). Insulin levels in insulin resistance: phantom of the metabolic opera? Medical Journal of Australia, 185(3)
- Garnett, S. P., Srinivasan, S., Birt, S. G., et al. (2010). Fasting insulin or OGTT in youth with risk features — insights from an Australian paediatric cohort. Clinical Endocrinology (Oxford).
- Li, M., Chi, X., Wang, Y., et al. (2022). Trends in insulin resistance: insights into mechanisms and therapeutic strategy. Signal Transduction and Targeted Therapy, 7, 216.
- Brogan, R. J., et al. (2025). Biomarkers of Insulin Resistance and Their Performance as Predictors of Response to Lifestyle Intervention. The Journal of Clinical Endocrinology & Metabolism.
















.png)


.svg)

