What is Mean Cell Haemoglobin (MCH)?
MCH stands for Mean Cell Haemoglobin (also sometimes called Mean Corpuscular Haemoglobin). It is a calculated laboratory parameter reflecting the average amount of haemoglobin in a single red blood cell (in picograms, pg). It is one of the red cell indices returned in a full blood or complete blood count.
Why does MCH matter for long-term health and wellbeing?
Although it is not a direct “performance marker,” MCH offers insight into how well your red cells are loaded with haemoglobin—and thus how efficiently oxygen can be carried. Over time, small inefficiencies in red cell oxygen delivery can influence fatigue, recovery, adaptation to training, metabolic flexibility, and cellular energy balance. By interpreting MCH in context (alongside MCV, red cell count, iron stores, B-vitamin markers, etc.), you gain a window into internal balance and can more proactively fine-tune your nutrition, cadence of recovery and micronutrient optimisation.
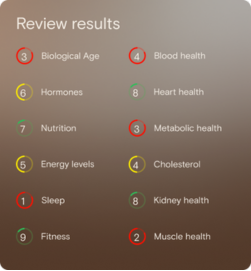
What’s an optimal level of MCH?
- Laboratory (reference) range: 26 to 34 pg
- Vively’s target (optimal) range: 27 to 33 pg
The laboratory reference range reflects what is considered “normal” across a broad population, whereas Vively’s optimal band is a narrower window aimed at better performance and resilience.
What influences MCH levels?
Many lifestyle and nutritional factors can influence MCH:
- Availability of iron (for haemoglobin synthesis)
- Availability of key cofactors such as vitamin B12, folate, vitamin B6
- Rates of red cell production and turnover
- Hydration status and plasma volume shifts
- Chronic inflammation or oxidative stress
- Nutrient absorption or losses (e.g. in the gut)
- Training load, recovery, and recovery stressors
- Genetic variance in haemoglobin synthesis or red cell machinery
Because it is downstream of multiple upstream inputs, MCH functions as an integrative readout of how well your nutritional, metabolic and cellular machinery is aligned.
What does it mean if MCH is outside the optimal range?
- Below 27 pg (low): It suggests that individual red cells may be under-loaded with haemoglobin, potentially because of limited iron supply, or suboptimal B-vitamin support. Over time, this could subtly erode your oxygen delivery reserve and contribute to feeling less energetic or slower recovery.
- Above 33 pg (high): While not necessarily problematic, elevated MCH may indicate shifts in red cell size or structure, possibly due to imbalances in B-vitamin metabolism or red cell turnover dynamics. It may also reflect compensatory adaptation (for example, fewer but larger red cells). Such deviations flag a signal to reassess upstream nutrition, recovery and micronutrient balance.
In both directions, a value outside the optimal window is not a diagnosis—rather, it is a prompt to explore upstream contributing factors and adjust your nutrition, recovery or lifestyle strategy.
How can I support healthy MCH levels?
Here are strategies (within a health-and-wellness framing) to nudge MCH toward your optimal zone:
- Ensure adequate iron intake via food sources rich in bioavailable iron (heme-iron sources, paired with vitamin C to aid absorption).
- Support B-vitamin status (B12, folate, B6) through diverse whole foods (leafy greens, legumes, lean protein, eggs, fortified foods)
- Manage training and recovery load so red cell demand and turnover remain sustainable
- Support gut health and absorption (healthy gut lining, moderate anti-inflammatory nutrition)
- Monitor hydration and plasma volume shifts, as changes in fluid balance influence red cell indices
- Track inflammation and oxidative stress, since chronic low-level inflammation can influence red cell synthesis
- Regularly retest and trend—monitor MCH alongside related red cell markers to see how your interventions move the dial
This information is provided for general health and wellness purposes only and does not replace medical advice.
References
- Healthdirect. Full blood count (FBC). Retrieved from Healthdirect Australia.
- Royal Children’s Hospital (Melbourne). Anaemia / red cell indices guidelines.
- Lifeblood. Diagnosis and investigation of iron deficiency anaemia.
- RCPA (Royal College of Pathologists of Australasia). Haemoglobin testing and red cell indices.

















.png)


.svg)

