What is the Neutrophil-to-Lymphocyte Ratio (NLR)?
NLR is a simple ratio — the number of neutrophils divided by the number of lymphocytes in the peripheral blood. Neutrophils act as the body’s first-responders to stress and inflammation, while lymphocytes drive the adaptive immune response. When one arm of this balance shifts relative to the other, NLR can move, signalling a shift in immune and inflammatory status.
Why does NLR matter for long-term health and wellbeing?
Maintaining a resilient immune system and low-grade inflammatory load are key to sustaining energy levels, efficient metabolism and healthy ageing. A stable, balanced NLR suggests your immune system is neither overly activated (which can drain resources) nor under-prepared. In contrast, shifts in NLR may indicate a need to adjust lifestyle inputs (sleep, nutrition, movement, stress) to keep your physiology primed for performance and recovery. Research shows NLR tracks immune-balance and inflammation across a wide range of contexts.
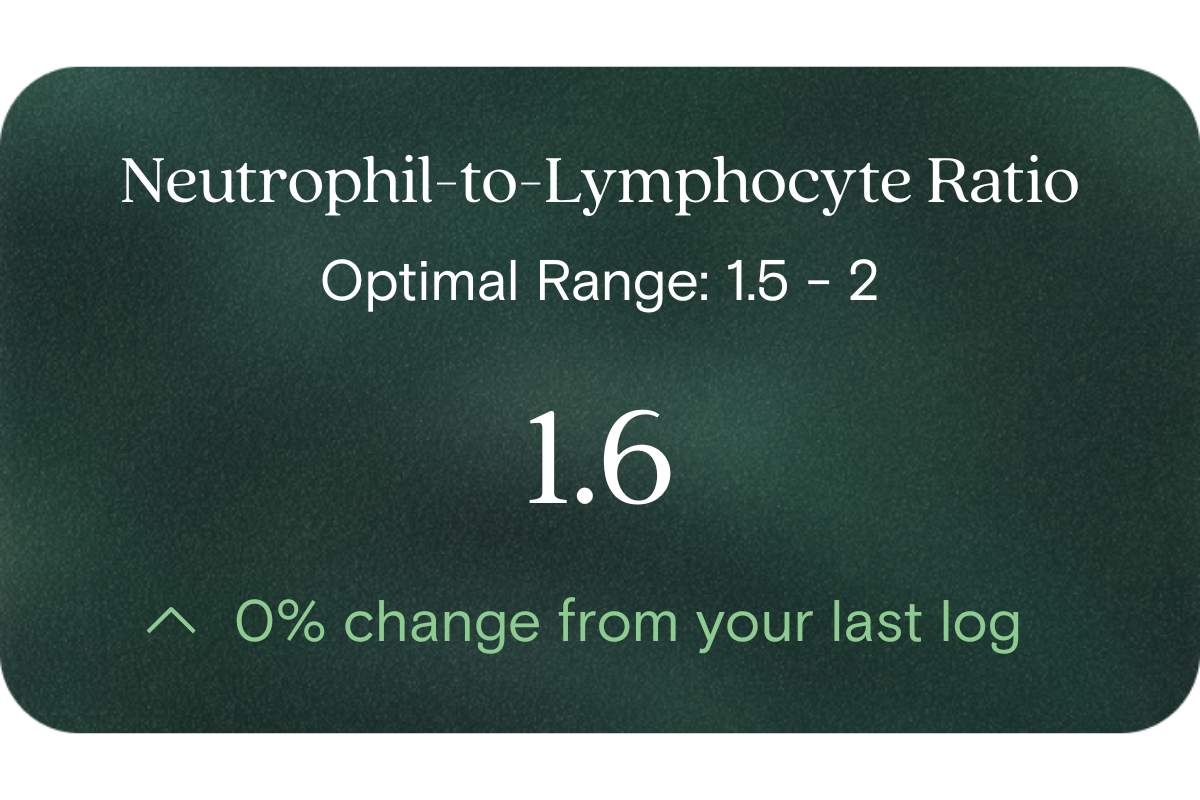
What’s an optimal level of NLR?
- Reference (lab) range: for healthy adults, typical values fall roughly between ~0.78 and ~3.53 (unitless ratio) in general populations.
- Optimal (for proactive health/performance) target: as a guideline, aiming for the lower end of that range (for example ~0.8–2.0) may indicate better immune-inflammatory balance.
- Example reference values (for Australians via standard blood counts):
- Reference range low: ~0.78
- Reference range high: ~3.5
- Optimal range low: ~0.8
- Optimal range high: ~2.0
Individual variation applies, including age, sex, ethnicity and lab method — so your baseline and trends matter most.
What influences NLR levels?
Several lifestyle and physiological factors may influence NLR, including:
- Acute physiological stress (e.g., intense exercise, surgery, sleep-deprivation) elevating neutrophils.
- Dietary quality, body-composition and metabolic load (which can modulate activity of immune cells).
- Sleep and recovery: poor sleep may drive elevated neutrophil counts and shift balance.
- Chronic stress or low-grade inflammation (e.g., from obesity, metabolic imbalance, environmental exposures).
- Ageing and immune-system adjustment: older individuals may show higher baseline NLR.
What does it mean if my NLR is outside the optimal range?
If your NLR is higher than your optimal target, it may signal that your immune-inflammatory balance is tilted toward elevated frontline activation (neutrophils) relative to adaptive capacity (lymphocytes). From a wellness-perspective this suggests your physiology may be under subtle stress, and that refining lifestyle inputs could help restore balance.
Conversely, if your NLR is lower than expected (though less commonly discussed), it might reflect an unusual shift in lymphocyte counts or immune responsiveness. In both cases the emphasis is on monitoring trend over time, not one isolated value, and using the result as an insight rather than a diagnosis.
How can I support healthy NLR levels?
To support a balanced NLR and therefore better immune-inflammatory balance:
- Prioritise restorative sleep (7–9 hours for most adults) and minimise chronic sleep deprivation.
- Use whole-food nutrition rich in anti-inflammatory nutrients (e.g., omega-3 fatty acids, colourful vegetables, fibre).
- Maintain regular physical activity combined with adequate recovery — over-training may elevate neutrophil counts.
- Manage stress (psychological, environmental, metabolic) through mindfulness, movement, social connection.
- Maintain healthy body composition, metabolic health and avoid excess adiposity, which can fuel low-grade inflammation.
- Monitor and optimise your other supporting biomarkers (e.g., sleep quality, resting heart-rate variability, nutrient status) to favour immune-balance.
This information is provided for general health and wellness purposes only and does not replace medical advice.
References
- Forget, P., Khalifa, C., Defour, J.-P., Latinne, D., Van Pel, A., De Kock, M. (2017). What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Research Notes, 10:12.
- Lee, J.-S., Im, J.-S., Lee, S.-H., et al. (2018). Reference values of neutrophil-lymphocyte ratio, platelet-lymphocyte ratio, and mean platelet volume in healthy children and adults. Medicine, 97(26):e11151.
- Arvanitakis, F., et al. (2023). The neutrophil-to-lymphocyte ratio as a new prognostic factor in cancers: narrative review. Frontiers in Oncology, 13:1228076.
- Pagánelli, R., et al. (2025). The neutrophil-to-lymphocyte ratio in aging and immunity. Exploration Immunology, Article 1003200.
















.png)


.svg)

