What is Neutrophils?
Neutrophils are a type of white blood cell (granulocyte) that plays an essential role in early defence against bacterial and fungal challenges. They are part of your innate immune system, often arriving first at sites of invasion or tissue stress, and are able to phagocytose (ingest) microbes, release antimicrobial compounds, and modulate inflammation via signalling (chemokines, cytokines). Their count is usually expressed as an absolute neutrophil count (ANC) in ×10⁹/L alongside the white cell differential.
Why does it matter for long-term health and wellbeing?
Because neutrophils are a frontline defence, their levels and behaviour reflect the “set point” of your immune vigilance. Chronically elevated neutrophil counts may indicate a low-grade inflammatory burden or stress on your immune system, which over time can influence metabolic regulation, repair processes, and tissue health. Conversely, persistently low counts can signal reduced resilience to microbial or systemic stressors. In either direction, those deviations serve as early warning signals—insights you can act on through lifestyle adjustments before downstream effects accumulate.
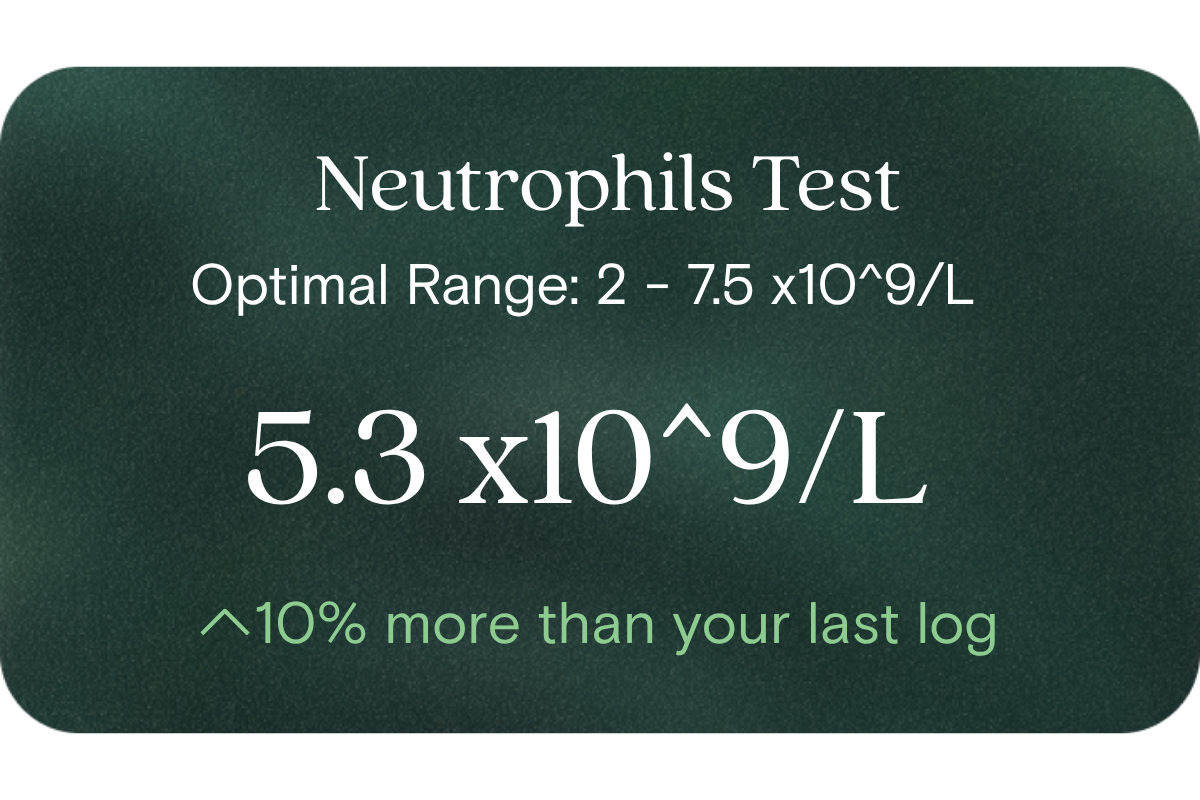
What’s an optimal level of Neutrophils?
- Common lab reference (population) range: ~ 2.0 to 7.5 ×10⁹/L (some labs use up to 8.0 ×10⁹/L)
- Suggested optimal window (for many healthy individuals): ~ 3.0 to 5.5 ×10⁹/L (this is a narrower target zone chosen for stability, minimal drift and good balance)
- Because “normal” ranges capture 95% of the population, your personal optimal may sit well inside that. Also, such targets should always be interpreted in the context of your trend, symptoms, and other immune/inflammatory markers.
What influences Neutrophils levels?
Several modifiable and non-modifiable factors can influence neutrophil counts:
- Acute stressors and infections: Transient rises in neutrophils often occur in response to bacterial challenge, tissue injury or inflammation.
- Physical exercise and training load: Intense or prolonged training may transiently shift white cell counts (including neutrophils).
- Nutrition and micronutrients: Deficiencies or imbalances (e.g. zinc, B vitamins, protein) may impair immune cell production.
- Sleep, circadian rhythms and recovery: Poor sleep or recovery cycles may dysregulate immune homeostasis.
- Chronic inflammation, oxidative stress and metabolic stress: Systemic stress burdens may gradually shift baseline neutrophil turnover.
- Genetic and demographic factors: Age, sex, ethnicity and inherited differences influence baseline counts and responsiveness.
What does it mean if Neutrophils is outside the optimal range?
- Above optimal (but within lab range): suggests your immune system may be under a low but persistent stressor (inflammatory burden, recovery lag, environmental or metabolic strain). It’s not a “disease” signal by itself—but a cue to reduce load, refine diet, support recovery or re-check trends.
- Below optimal (but within lab range): could reflect suppressed bone marrow function, nutritional constraints, overrecovery, or other stressors pulling down immune production. Again, it’s a signal to evaluate recovery status, nutrient density, sleep and immune load.
- If the value lies outside the lab’s reference range, especially if sustained across multiple tests, this amplifies the need for deeper evaluation—but even then, your trend and lifestyle context remain crucial to interpret meaningfully.
How can I support healthy Neutrophils levels?
You can take several evidence-backed steps to support robust neutrophil balance:
- Prioritise nutrient adequacy: Ensure sufficient protein, zinc, vitamins B6, B12, folate, magnesium and antioxidants through whole food diet or guided supplementation.
- Manage training load and recovery: Periodise exercise, avoid chronic overload without rest, incorporate deloads and active recovery.
- Get consistent sleep and circadian rhythms: Aim for quality sleep (7–9 h), maintain consistent sleep–wake times, and reduce late night stressors.
- Minimise chronic stressors: Use stress management techniques (mindfulness, breathwork, nature exposure) to lessen chronic immune activation.
- Support gut and immune health: Ensure fibre, prebiotics, probiotics or microbiome-friendly diet, because gut–immune signalling influences neutrophil production and trafficking.
- Monitor and adjust over time: Repeat testing and trend analysis allow you to catch drift early and test the impact of interventions.
This information is provided for general health and wellness purposes only and does not replace medical advice.
References
- Von Vietinghoff, S., Ley, K. (2008). Homeostatic regulation of blood neutrophil counts. Journal of Immunology / PMC.
- Best Practice Advocacy Centre (bpac). “Complete Blood Count in Primary Care” (Neutrophil range discussion).
- “Neutrophil (Wikipedia)” – normal ranges, physiology summary.
- ODX Research “Biomarkers of Immunity: Neutrophils” (optimal ranges discussion)
















.png)


.svg)

