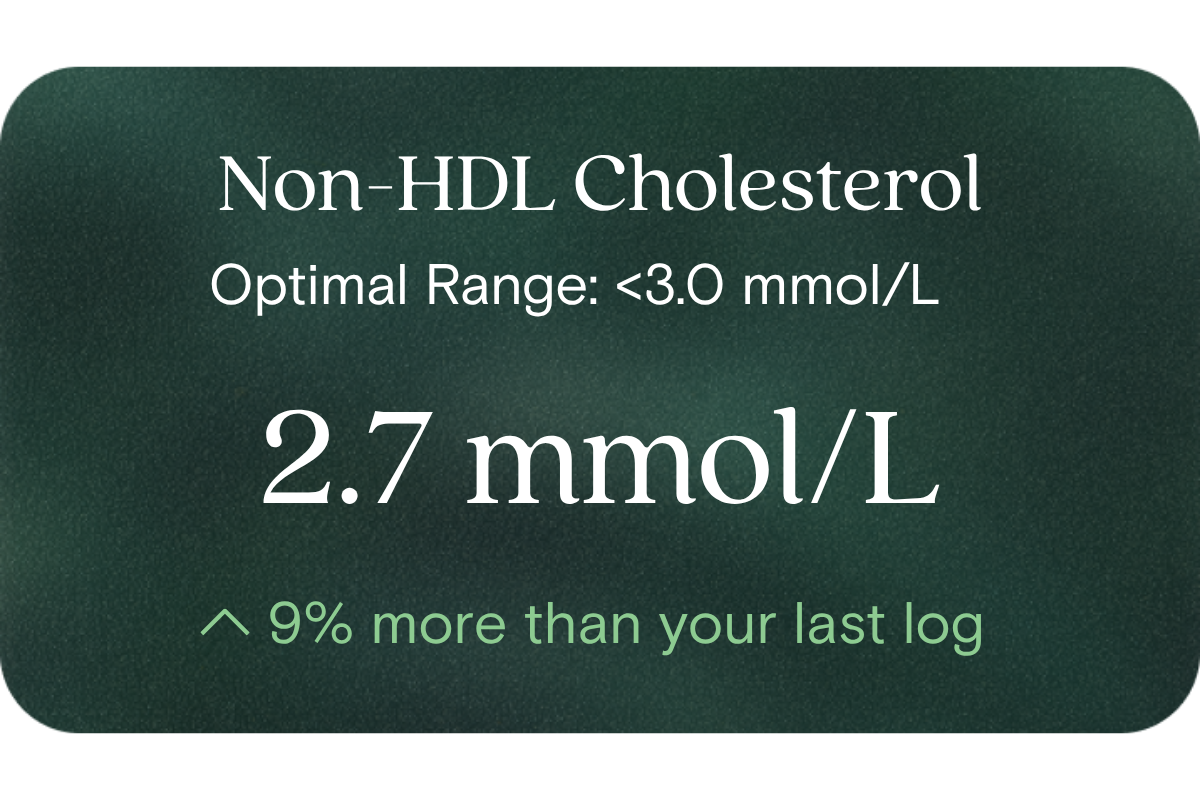
What is Non-HDL Cholesterol?
Non-HDL cholesterol is the cholesterol content of all the lipoproteins besides HDL. In other words, it is your total cholesterol minus HDL-C. Because it includes LDL, VLDL, IDL, and remnants, it captures the full “bad” cholesterol burden transported in your bloodstream.
Why does it matter for long-term health and wellbeing?
Non-HDL is considered a stronger predictor of long-term vascular and metabolic strain than LDL or simple cholesterol ratios alone, because it aggregates all atherogenic particles. High non-HDL levels often align with underlying metabolic inefficiencies (e.g. insulin resistance, dysregulated lipid metabolism). By proactively monitoring it, you gain feedback on how your lifestyle, diet, exercise and body composition are influencing your core metabolic health — long before overt issues arise.
What’s an optimal level of Non-HDL Cholesterol?
- Optimal (target for performance/health optimisation): < 3.0 mmol/L
- Lab / reference high threshold: 3.4 mmol/L
These targets place you in a zone of lower atherogenic burden and greater metabolic headroom. (By comparison, some pathology labs and guidelines in Australia consider < 3.8 mmol/L or < 3.3 mmol/L in certain risk tiers as desirable bounds)
What influences Non-HDL Cholesterol levels?
- Dietary fats (particularly saturated and trans fats)
- Refined carbohydrate and sugar load
- Body fat distribution (especially visceral adiposity)
- Insulin sensitivity / glucose metabolism
- Physical activity / aerobic and resistance training
- Genetic lipid handling (lipoprotein production, clearance)
- Sleep, stress, and inflammatory status
- Alcohol intake, cigarette exposure, and other lifestyle modifiers
What does it mean if Non-HDL is outside the optimal range?
If your non-HDL is elevated (above ~3.0 mmol/L or exceeding your lab’s reference high), it signals a greater cumulative lipid burden on your vascular and metabolic system. It suggests that your lifestyle inputs (diet, movement, body composition) aren’t sufficiently offsetting lipid stress. That is not a “disease,” but a signal that your system is under pressure — and that further optimisation or course correction may yield more resilience, energy, and long-term robustness.
How can I support healthy Non-HDL Cholesterol levels?
- Emphasise whole foods and reduce saturated and trans fats; favour monounsaturated and polyunsaturated sources
- Increase soluble fibre (e.g. oats, legumes, psyllium)
- Moderate refined carbs and added sugars
- Build consistent aerobic and resistance exercise habits
- Aim for healthy body composition, especially reducing visceral fat
- Support insulin sensitivity with strategic nutrition timing, resistance training, and sleep hygiene
- Manage stress, minimise alcohol excess, avoid tobacco
- Monitor your progress over time so you can adapt strategies before drift accumulates
This information is provided for general health and wellness purposes only and does not replace medical advice.
References
- Hickman PE, Ashby MA, Beilby JP, et al. Recommendations for Lipid Testing and Reporting. Pathology. 2007.
- Carr SS, et al. “Non-HDL-cholesterol and apolipoprotein B compared with LDL-cholesterol in atherosclerotic cardiovascular disease risk assessment.” Pathology 2019
- Royal College of Pathologists of Australasia. Non-HDL cholesterol — RCPA Manual.
















.png)


.svg)

