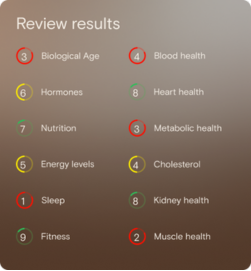
What is Total Testosterone?
A testosterone blood test measures total testosterone, which includes free testosterone and testosterone bound to albumin and SHBG, providing an overview of overall testosterone availability in the body in nmol/L.
Why does it matter for long-term health and wellbeing?
Total testosterone supports physical strength, bone integrity, energy balance, libido, mental focus, and healthy ageing, making it a valuable marker for monitoring performance and resilience across life stages.
What’s an optimal level of Total Testosterone?
For females, the typical laboratory reference range is 0.5–3.2 nmol/L, with an optimal range often considered around 1.5–3.2 nmol/L.
For males, the laboratory reference range is approximately 11–40 nmol/L, with levels above around 12 nmol/L commonly viewed as supportive of optimal function, depending on individual context.
What influences Total Testosterone levels?
Levels are influenced by age, body composition, physical activity, sleep quality, stress, alcohol intake, nutrition, insulin sensitivity, supplements, and timing of testing. In men, levels follow a daily rhythm and are best measured in the early morning, while in women timing within the menstrual cycle can affect results.
What does it mean if Total Testosterone is outside the optimal range?
Values outside the optimal range may indicate that lifestyle, recovery, or metabolic factors are placing extra demand on the body. These insights can help guide adjustments to training, nutrition, sleep, or stress management to better support balance and performance.
How can I support healthy Total Testosterone levels?
Supporting healthy levels often involves quality sleep, balanced nutrition, regular resistance and aerobic exercise, stress management, moderated alcohol intake, and a healthy body composition. Using an at home testosterone test makes it easier to track trends over time and see how these lifestyle choices influence results.
This information is provided for general health and wellness purposes only and does not replace medical advice.
References
- Grossmann, M., & Matsumoto, A. M. (2017). A perspective on middle-aged and older men with functional hypogonadism: Focus on holistic management. Journal of Clinical Endocrinology & Metabolism, 102(3), 1067–1075.
- Yeap, B. B., Grossmann, M., McLachlan, R. I., Conway, A. J., Handelsman, D. J., & Wittert, G. A. (2016). Endocrine Society of Australia position statement on male hypogonadism (Part 1): Assessment. Medical Journal of Australia, 205(4), 173–178.
- Perry-Keene, D. (2014). Low testosterone in men. Australian Prescriber, 37(4), 124–127.
.png)
















.png)


.svg)

