Choose how you’d like to begin
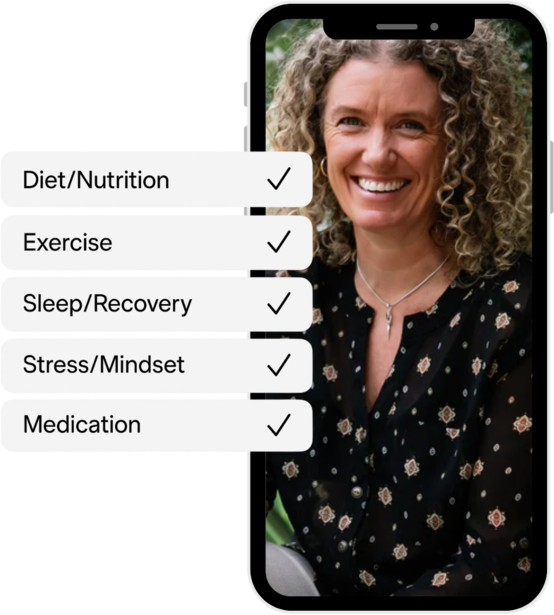
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan



Delve into the significant role that glucose regulation plays during menopause. Understand the implications of glucose on metabolic health and how to manage it for optimal health.
Menopause, marking the end of a woman's menstrual cycle, is a period of significant physiological transformation. It's not just about hot flushes and the cessation of monthly periods. The changes occurring on a cellular level can greatly impact a woman's daily experience and future health.
Stabilising glucose levels is a fundamental aspect of good health. The more stable your glucose levels, the more balanced your energy levels, inflammatory chemicals, and insulin levels become.
During menopause, the production of hormones such as oestrogen and progesterone declines significantly. These hormones are believed to help regulate insulin, the hormone that regulates blood sugar levels. When levels of oestrogen and progesterone drop, this can disrupt insulin regulation, leading to increased blood sugar levels and greater insulin resistance.
Additionally, menopause is often accompanied by changes in body weight and composition, with many women experiencing weight gain and an increase in abdominal fat. This type of fat is linked to insulin resistance and higher blood sugar levels.
Symptoms associated with menopause such as hot flashes and night sweats can cause sleep disturbances, leading to poor sleep quality. Lack of sleep has been linked to impaired glucose metabolism and increased insulin resistance. Along with sleep disturbances, the stress associated with menopause can result in high blood sugar levels. When a person is stressed, their body releases stress hormones like cortisol, which can cause blood sugar levels to rise.
A woman's risk of certain diseases increases significantly during menopause. Oestrogen and progesterone, which are thought to protect against metabolic syndrome, cardiovascular disease, and cognitive issues, decrease during menopause. Consequently, women's rates of cardiovascular disease increase significantly when these hormonal safeguards are no longer present. In fact, heart disease is the most common cause of death in post-menopausal women.
With the fluctuation of glucose levels in menopause, resting and post-prandial insulin levels can increase. Over time, if left untreated or poorly controlled, this can result in type 2 diabetes. Individuals with type 2 diabetes face an increased risk of health issues, including heart attack, limb amputation, blindness, cancer, dementia, and nerve damage. This underlines the importance of glucose regulation for both the short and long-term health.
Maintaining good metabolic health becomes more challenging after menopause. Women often experience a shift in weight distribution, have difficulty losing weight, become more prone to injury, and feel sleep deprived. All these factors heighten the risk of glucose dysregulation.
To understand how your glucose levels fair, your doctor may recommend a HbA1c test. This test checks your average glucose over a three-month period. While this is an excellent measure to ensure you're not diabetic, it doesn't account for excessive glucose variability.
Glucose variability measures the highs and lows of your blood sugar levels. If your glucose readings fluctuate significantly (high variability), it can lead to misleading average glucose levels. Similarly, fasting glucose readings might not identify high glucose variability either.
Continuous glucose monitors (CGMs) can be a great option to help you manage your blood sugar levels during menopause. CGMs provide real-time, detailed information on blood glucose levels throughout the day and night. They offer a more comprehensive picture of glucose variations, capturing not just the highs and lows, but also how quickly these changes occur.
For women going through menopause, who may experience increased insulin resistance and fluctuating blood sugar levels due to hormonal changes, a CGM can be invaluable. It can help identify specific times or events that cause glucose spikes, such as certain meals or periods of stress. This data can then be used to make informed decisions about diet, exercise, and other lifestyle adjustments to better manage glucose levels and overall health during menopause.
Achieving balanced glucose levels can have wide-ranging positive effects on health. It can lower inflammation, reduce stress, optimise energy, and support a woman's system throughout this incredible natural process. Furthermore, better glucose control can help mitigate some menopausal symptoms and reduce the risk of developing complications such as type 2 diabetes and cardiovascular diseases.
Taking the initial step towards improving your health during menopause can start with simple dietary modifications. Specifically, reducing your consumption of sugar, alcohol, and caffeine can be a powerful first move. These substances are known to cause fluctuations in blood glucose levels and can contribute to feelings of fatigue, mood swings, and other menopausal symptoms.
By reducing these factors, you might notice a significant stabilisation in both your energy levels and blood glucose. This reduction not only supports your body's natural glucose regulation mechanisms but also can lead to a more consistent energy output throughout the day. Consequently, this can provide you with an additional energy boost that motivates you to engage in outdoor activities or regular exercise.
Regular physical activity is known to improve insulin sensitivity and glucose regulation, creating a positive feedback loop in your health management. Furthermore, physical activity can also promote better mood, improved muscle mass, weight loss/management, and overall well being during menopause.
Improved sleep patterns often coincide with these lifestyle adjustments. Good sleep is essential for glucose metabolism and hormone regulation. Disrupted sleep, a common complaint during menopause, can aggravate menopausal symptoms and contribute to glucose dysregulation. Therefore, improvements in diet and exercise often result in more restful sleep, further supporting the body's ability to manage glucose and other physiological changes associated with menopause.
Maintaining balanced glucose levels is not just about managing menopause weight gain, it's also a preventative measure against other health implications. Implementing changes in your lifestyle can contribute significantly to menopause treatment, not only by alleviating physical symptoms but also by boosting your mood and overall well being.
It's always advised to consult with your doctor before making changes to your diet or lifestyle. Everyone's body responds differently, and a tailored approach based on your individual needs will yield the best results. In the end, menopause is a natural phase in life. With the right understanding and management of glucose levels, it can be navigated with grace and positivity.
Vively is a metabolic health app that uses CGMs to help women improve their glucose levels and in turn their menopause symptoms. The app uses glucose tracking, education and support to help improve your lifestyle and overall quality of life.
Bermingham, K. M., Linenberg, I., Hall, W. L., Kadé, K., Franks, P. W., Davies, R., ... & et al. (2022). Menopause is associated with postprandial metabolism, metabolic health and lifestyle: The ZOE PREDICT study. EBioMedicine. https://doi.org/10.1016/j.ebiom.2022.104303
Martinez, M., Santamarina, J., Pavesi, A., et al. (2021). Glycemic variability and cardiovascular disease in patients with type 2 diabetes. BMJ Open Diabetes Research and Care, 9, e002032. https://doi.org/10.1136/bmjdrc-2020-002032
Otsuki, M., Kasayama, S., Morita, S., Asanuma, N., Saito, H., Mukai, M., & Koga, M. (2007). Menopause, but not age, is an independent risk factor for fasting plasma glucose levels in nondiabetic women. Menopause, 14(3 Pt 1), 404-407. https://doi.org/10.1097/01.gme.0000247014.56254.12
Subscribe to our newsletter & join a community of 20,000+ Aussies

Delve into the significant role that glucose regulation plays during menopause. Understand the implications of glucose on metabolic health and how to manage it for optimal health.
Menopause, marking the end of a woman's menstrual cycle, is a period of significant physiological transformation. It's not just about hot flushes and the cessation of monthly periods. The changes occurring on a cellular level can greatly impact a woman's daily experience and future health.
Stabilising glucose levels is a fundamental aspect of good health. The more stable your glucose levels, the more balanced your energy levels, inflammatory chemicals, and insulin levels become.
During menopause, the production of hormones such as oestrogen and progesterone declines significantly. These hormones are believed to help regulate insulin, the hormone that regulates blood sugar levels. When levels of oestrogen and progesterone drop, this can disrupt insulin regulation, leading to increased blood sugar levels and greater insulin resistance.
Additionally, menopause is often accompanied by changes in body weight and composition, with many women experiencing weight gain and an increase in abdominal fat. This type of fat is linked to insulin resistance and higher blood sugar levels.
Symptoms associated with menopause such as hot flashes and night sweats can cause sleep disturbances, leading to poor sleep quality. Lack of sleep has been linked to impaired glucose metabolism and increased insulin resistance. Along with sleep disturbances, the stress associated with menopause can result in high blood sugar levels. When a person is stressed, their body releases stress hormones like cortisol, which can cause blood sugar levels to rise.
A woman's risk of certain diseases increases significantly during menopause. Oestrogen and progesterone, which are thought to protect against metabolic syndrome, cardiovascular disease, and cognitive issues, decrease during menopause. Consequently, women's rates of cardiovascular disease increase significantly when these hormonal safeguards are no longer present. In fact, heart disease is the most common cause of death in post-menopausal women.
With the fluctuation of glucose levels in menopause, resting and post-prandial insulin levels can increase. Over time, if left untreated or poorly controlled, this can result in type 2 diabetes. Individuals with type 2 diabetes face an increased risk of health issues, including heart attack, limb amputation, blindness, cancer, dementia, and nerve damage. This underlines the importance of glucose regulation for both the short and long-term health.
Maintaining good metabolic health becomes more challenging after menopause. Women often experience a shift in weight distribution, have difficulty losing weight, become more prone to injury, and feel sleep deprived. All these factors heighten the risk of glucose dysregulation.
To understand how your glucose levels fair, your doctor may recommend a HbA1c test. This test checks your average glucose over a three-month period. While this is an excellent measure to ensure you're not diabetic, it doesn't account for excessive glucose variability.
Glucose variability measures the highs and lows of your blood sugar levels. If your glucose readings fluctuate significantly (high variability), it can lead to misleading average glucose levels. Similarly, fasting glucose readings might not identify high glucose variability either.
Continuous glucose monitors (CGMs) can be a great option to help you manage your blood sugar levels during menopause. CGMs provide real-time, detailed information on blood glucose levels throughout the day and night. They offer a more comprehensive picture of glucose variations, capturing not just the highs and lows, but also how quickly these changes occur.
For women going through menopause, who may experience increased insulin resistance and fluctuating blood sugar levels due to hormonal changes, a CGM can be invaluable. It can help identify specific times or events that cause glucose spikes, such as certain meals or periods of stress. This data can then be used to make informed decisions about diet, exercise, and other lifestyle adjustments to better manage glucose levels and overall health during menopause.
Achieving balanced glucose levels can have wide-ranging positive effects on health. It can lower inflammation, reduce stress, optimise energy, and support a woman's system throughout this incredible natural process. Furthermore, better glucose control can help mitigate some menopausal symptoms and reduce the risk of developing complications such as type 2 diabetes and cardiovascular diseases.
Taking the initial step towards improving your health during menopause can start with simple dietary modifications. Specifically, reducing your consumption of sugar, alcohol, and caffeine can be a powerful first move. These substances are known to cause fluctuations in blood glucose levels and can contribute to feelings of fatigue, mood swings, and other menopausal symptoms.
By reducing these factors, you might notice a significant stabilisation in both your energy levels and blood glucose. This reduction not only supports your body's natural glucose regulation mechanisms but also can lead to a more consistent energy output throughout the day. Consequently, this can provide you with an additional energy boost that motivates you to engage in outdoor activities or regular exercise.
Regular physical activity is known to improve insulin sensitivity and glucose regulation, creating a positive feedback loop in your health management. Furthermore, physical activity can also promote better mood, improved muscle mass, weight loss/management, and overall well being during menopause.
Improved sleep patterns often coincide with these lifestyle adjustments. Good sleep is essential for glucose metabolism and hormone regulation. Disrupted sleep, a common complaint during menopause, can aggravate menopausal symptoms and contribute to glucose dysregulation. Therefore, improvements in diet and exercise often result in more restful sleep, further supporting the body's ability to manage glucose and other physiological changes associated with menopause.
Maintaining balanced glucose levels is not just about managing menopause weight gain, it's also a preventative measure against other health implications. Implementing changes in your lifestyle can contribute significantly to menopause treatment, not only by alleviating physical symptoms but also by boosting your mood and overall well being.
It's always advised to consult with your doctor before making changes to your diet or lifestyle. Everyone's body responds differently, and a tailored approach based on your individual needs will yield the best results. In the end, menopause is a natural phase in life. With the right understanding and management of glucose levels, it can be navigated with grace and positivity.
Vively is a metabolic health app that uses CGMs to help women improve their glucose levels and in turn their menopause symptoms. The app uses glucose tracking, education and support to help improve your lifestyle and overall quality of life.
Bermingham, K. M., Linenberg, I., Hall, W. L., Kadé, K., Franks, P. W., Davies, R., ... & et al. (2022). Menopause is associated with postprandial metabolism, metabolic health and lifestyle: The ZOE PREDICT study. EBioMedicine. https://doi.org/10.1016/j.ebiom.2022.104303
Martinez, M., Santamarina, J., Pavesi, A., et al. (2021). Glycemic variability and cardiovascular disease in patients with type 2 diabetes. BMJ Open Diabetes Research and Care, 9, e002032. https://doi.org/10.1136/bmjdrc-2020-002032
Otsuki, M., Kasayama, S., Morita, S., Asanuma, N., Saito, H., Mukai, M., & Koga, M. (2007). Menopause, but not age, is an independent risk factor for fasting plasma glucose levels in nondiabetic women. Menopause, 14(3 Pt 1), 404-407. https://doi.org/10.1097/01.gme.0000247014.56254.12
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
