Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan



Your glucose and insulin control are associated with your weight. Tracking your glucose levels can be a fantastic weight loss tool. Read on to learn more about how this can help you.
Research shows that 60% of Australians are trying to lose weight, and only 15% are sustainably successful. The fact is that restrictive diets rarely prevail.
Maintaining a healthy weight was simpler thousands of years ago. Our bodies held onto energy due to the risk of famine. We were engineered to seek fast-acting energy sources like sugar. Food was harder to come by, and people walked incredible distances daily.
This is no longer the case in our current society. Modern-day farming, our sedentary lifestyle and convenience foods has resulted in many people struggling to maintain a healthy weight.
The traditional weight loss model of ‘calories in versus calories out’ assumes the way you metabolise food is always the same. However, your hormonal regulatory systems, detoxification, structural differences and inflammatory requirements make metabolism and weight loss much more complex.
Simplifying weight loss to purely calorie deprivation can be detrimental in many ways. Calorie deprivation can actually thwart weight loss efforts by reducing your resting metabolic rate. When the body senses a food shortage risk, it becomes more energy efficient by reducing the usage of stored fat.
Not only that, but when the brain experiences calorie restriction, the areas for attention, reward and motivation are stimulated. This makes you more food-focused. Not to mention the negative effects calorie restriction can have on mental health.
Looking at weight loss more holistically is important. Understanding more about your unique metabolism can empower you to make positive changes that suit you.
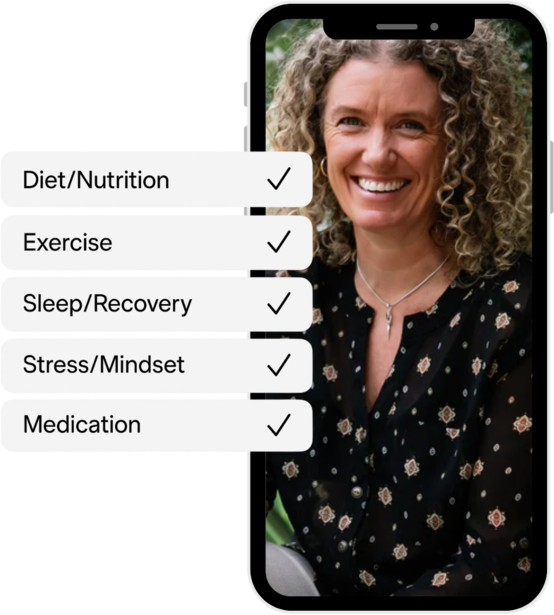
The way you metabolise food will depend upon your:
Lifestyle factors are also extremely important in determining how you metabolise food. This includes your food sources, food combinations and timing of meals.
Carrying excess weight, poor sleep, sedentary behaviour, alcohol overconsumption and environmental disruptors also contribute to dysregulating adaptive hormonal responses. This may lead to chronic low-grade inflammation. All of which can contribute to weight gain.
Insulin is the key messenger in glucose regulation. It is secreted from the pancreas in response to high blood sugar levels. When your glucose levels rise, your insulin levels do the same. If they are consistently high, the cells become less insulin sensitive, leading to insulin resistance.
When there is an excess of glucose, the liver and muscles store it for later use. Once the storage is at capacity, the remaining glucose gets converted into fat, contributing to weight gain.
This fat is delivered to the tissues in the form of triglycerides. Blood triglyceride levels are an indicator of metabolic health. Whilst the storage in the liver and muscles is finite, the storage capacity for fat is almost insatiable.
During sleep or when you skip a meal, the lack of glucose intake decreases insulin levels. This signals the body to use up the glycogen stores. When depleted, the body then burns fat as fuel.
However, if the insulin levels remain high, like in insulin resistance, the body can’t use the stored fat for energy. In addition, insulin blocks the body’s ability to break down triglycerides. This prevents fatty acids from being used as energy. Therefore, low insulin levels are needed to burn fat and result in weight loss.
Another associated hormone is leptin. Leptin is associated with appetite and satiety. It is made and released by fat cells. It manages how many calories are consumed to regulate energy requirements.
The more fat cells you have and the more insulin that is made, the more leptin resistant you become. This means despite having sufficient fat, you still feel hungry, which perpetuates the cycle.
Managing your blood glucose levels can have a positive effect on insulin, as insulin mirrors glucose. When the amount of insulin is normal, cells can burn fat more effectively. This can lead to sustained weight loss if managed long-term. It's important to aim for low glucose variability (steady levels) and tight control within the target range.
Using a continuous glucose monitor (CGM) can reveal your glucose responses to food to help with weight management long-term. The more you can understand your unique metabolism, the more you can make healthy choices that suit you. Unlike traditional means like calorie tracking, measuring glucose can be impactful for witnessing the physiological effects of food and lifestyle choices.
If you’re on this journey, you might feel that a low carbohydrate diet plan is the only way forward. However, using a CGM can help you manage your carbohydrate intake in ways other than restriction (which is best to avoid). It’s important that your diet is diverse, socially inclusive and enjoyable.
Experimenting with carbohydrates in certain combinations, portions and times of the day can vary your glucose response. For example, a higher carb meal in the evening may produce a greater glucose and insulin spike compared to the morning.
The order you eat your foods can also change your glucose response. When carbohydrates are eaten first, your glucose spikes may be higher than if you ate your carbohydrates last. Same meal composition, different timing, different physiological response.
It's important to note that everyone's metabolism is different. A 2007 study on a group of non-diabetic people found differences in glucose responses between individuals for the same meals. Evidence also shows that the same person can have a different glucose response to the same carbohydrate load.
In conclusion, stabilising your glucose and insulin in conjunction with healthy lifestyle changes can be a really positive step towards optimal metabolic health. CGMs can be a fantastic tool to help with this. It’s important to seek advice from your doctor if you’re unsure if a CGM will work for you.
At Vively, we try to understand the drivers of chronic disease, including obesity and hyper-insulinaemia. Using CGM devices to unlock personalised insights can be a game changer for sustainable wellness.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Your glucose and insulin control are associated with your weight. Tracking your glucose levels can be a fantastic weight loss tool. Read on to learn more about how this can help you.
Research shows that 60% of Australians are trying to lose weight, and only 15% are sustainably successful. The fact is that restrictive diets rarely prevail.
Maintaining a healthy weight was simpler thousands of years ago. Our bodies held onto energy due to the risk of famine. We were engineered to seek fast-acting energy sources like sugar. Food was harder to come by, and people walked incredible distances daily.
This is no longer the case in our current society. Modern-day farming, our sedentary lifestyle and convenience foods has resulted in many people struggling to maintain a healthy weight.
The traditional weight loss model of ‘calories in versus calories out’ assumes the way you metabolise food is always the same. However, your hormonal regulatory systems, detoxification, structural differences and inflammatory requirements make metabolism and weight loss much more complex.
Simplifying weight loss to purely calorie deprivation can be detrimental in many ways. Calorie deprivation can actually thwart weight loss efforts by reducing your resting metabolic rate. When the body senses a food shortage risk, it becomes more energy efficient by reducing the usage of stored fat.
Not only that, but when the brain experiences calorie restriction, the areas for attention, reward and motivation are stimulated. This makes you more food-focused. Not to mention the negative effects calorie restriction can have on mental health.
Looking at weight loss more holistically is important. Understanding more about your unique metabolism can empower you to make positive changes that suit you.
The way you metabolise food will depend upon your:
Lifestyle factors are also extremely important in determining how you metabolise food. This includes your food sources, food combinations and timing of meals.
Carrying excess weight, poor sleep, sedentary behaviour, alcohol overconsumption and environmental disruptors also contribute to dysregulating adaptive hormonal responses. This may lead to chronic low-grade inflammation. All of which can contribute to weight gain.
Insulin is the key messenger in glucose regulation. It is secreted from the pancreas in response to high blood sugar levels. When your glucose levels rise, your insulin levels do the same. If they are consistently high, the cells become less insulin sensitive, leading to insulin resistance.
When there is an excess of glucose, the liver and muscles store it for later use. Once the storage is at capacity, the remaining glucose gets converted into fat, contributing to weight gain.
This fat is delivered to the tissues in the form of triglycerides. Blood triglyceride levels are an indicator of metabolic health. Whilst the storage in the liver and muscles is finite, the storage capacity for fat is almost insatiable.
During sleep or when you skip a meal, the lack of glucose intake decreases insulin levels. This signals the body to use up the glycogen stores. When depleted, the body then burns fat as fuel.
However, if the insulin levels remain high, like in insulin resistance, the body can’t use the stored fat for energy. In addition, insulin blocks the body’s ability to break down triglycerides. This prevents fatty acids from being used as energy. Therefore, low insulin levels are needed to burn fat and result in weight loss.
Another associated hormone is leptin. Leptin is associated with appetite and satiety. It is made and released by fat cells. It manages how many calories are consumed to regulate energy requirements.
The more fat cells you have and the more insulin that is made, the more leptin resistant you become. This means despite having sufficient fat, you still feel hungry, which perpetuates the cycle.
Managing your blood glucose levels can have a positive effect on insulin, as insulin mirrors glucose. When the amount of insulin is normal, cells can burn fat more effectively. This can lead to sustained weight loss if managed long-term. It's important to aim for low glucose variability (steady levels) and tight control within the target range.
Using a continuous glucose monitor (CGM) can reveal your glucose responses to food to help with weight management long-term. The more you can understand your unique metabolism, the more you can make healthy choices that suit you. Unlike traditional means like calorie tracking, measuring glucose can be impactful for witnessing the physiological effects of food and lifestyle choices.
If you’re on this journey, you might feel that a low carbohydrate diet plan is the only way forward. However, using a CGM can help you manage your carbohydrate intake in ways other than restriction (which is best to avoid). It’s important that your diet is diverse, socially inclusive and enjoyable.
Experimenting with carbohydrates in certain combinations, portions and times of the day can vary your glucose response. For example, a higher carb meal in the evening may produce a greater glucose and insulin spike compared to the morning.
The order you eat your foods can also change your glucose response. When carbohydrates are eaten first, your glucose spikes may be higher than if you ate your carbohydrates last. Same meal composition, different timing, different physiological response.
It's important to note that everyone's metabolism is different. A 2007 study on a group of non-diabetic people found differences in glucose responses between individuals for the same meals. Evidence also shows that the same person can have a different glucose response to the same carbohydrate load.
In conclusion, stabilising your glucose and insulin in conjunction with healthy lifestyle changes can be a really positive step towards optimal metabolic health. CGMs can be a fantastic tool to help with this. It’s important to seek advice from your doctor if you’re unsure if a CGM will work for you.
At Vively, we try to understand the drivers of chronic disease, including obesity and hyper-insulinaemia. Using CGM devices to unlock personalised insights can be a game changer for sustainable wellness.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
