Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan



Delve into an informative guide to understanding insulin resistance – its causes, signs and symptoms, testing methods, and how to effectively prevent it.
The term insulin resistance, also known as impaired insulin sensitivity, is often associated with prediabetes and type 2 diabetes. However, anyone can develop it, particularly if they lead a sedentary lifestyle or do not maintain a balanced diet. Even individuals without diabetes can experience this condition. If not managed effectively, impaired insulin sensitivity can progress to type 2 diabetes.
Insulin plays an essential role in your body's performance beyond regulating blood glucose levels. It allows blood sugar to enter cells for energy and tells the liver to store glucose for later use. It is necessary for the metabolism of carbohydrates, lipids, and proteins, which drives cell growth and provides the body with energy.
Impaired insulin sensitivity means that your body isn't utilising insulin effectively. This inefficiency requires a higher level of insulin to deliver glucose to fat and muscle cells.
The pancreas attempts to compensate by producing more insulin, to allow the glucose to enter the cells. However, the pancreatic cells that produce insulin can quickly deteriorate. When this happens, high blood sugar levels occur, increasing your risk for type 2 diabetes or prediabetes.
It can also lead to metabolic syndrome, heightening the risk of heart disease, kidney disease, obesity, polycystic ovary syndrome (PCOS), non-alcoholic fatty liver disease, among other conditions.
Insulin resistance symptoms may not be apparent in some people because their pancreas can still increase the body's insulin level to avoid excessive glucose in the bloodstream. However, with more significant insulin resistance, individuals may experience symptoms such as:
If you are experiencing these symptoms or are concerned, please speak with your healthcare professional.
To diagnose insulin resistance, healthcare professionals evaluate various aspects of a patient's health, including:
In terms of testing, the tests generally assess your blood glucose levels. Some of the most common insulin resistance tests in Australia include:

Keep in mind that the normal levels for these tests may vary. It's important to seek the guidance of your doctor for interpreting your test results.
Some individuals may also be asked to do a blood test to assess their lipids. These blood tests often measure triglycerides, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and total cholesterol. People with insulin resistance often have high triglyceride and low HDL levels as well as high levels of blood sugar.
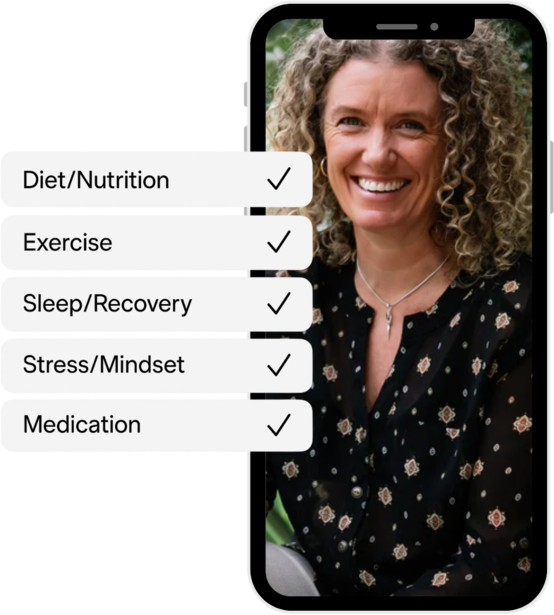
The primary objective when managing insulin resistance is to restore your body's sensitivity to insulin, and stabilise your glucose levels so that cells can efficiently absorb glucose. Several lifestyle adjustments can help improve insulin sensitivity and reverse insulin resistance:
Some individuals may require medication to help manage their blood sugar. Discuss options with your doctor to determine a suitable insulin resistance management plan.
Continuous glucose monitoring (CGM) helps track blood sugar levels in real time. It provides valuable insights into how food, exercise, and daily habits affect glucose levels. For those managing insulin resistance, CGM can make a big difference in understanding patterns and making better decisions.
A small sensor placed under the skin measures glucose levels throughout the day. The data is sent to a device or smartphone app, showing trends and spikes in real time. This helps identify how meals or activities impact blood sugar.
Regularly reviewing CGM data with a doctor or dietitian can help create a tailored plan. Adjustments to meals, exercise, or medication can improve insulin sensitivity. Over time, these changes may lower the risk of type 2 diabetes.
Adding CGM to your health routine makes managing insulin resistance easier. It provides continuous feedback, making it a helpful tool for long-term success.
Early action is key to managing insulin resistance and reducing the risk of type 2 diabetes. Understanding its causes, symptoms, and testing options helps in making informed choices. Simple steps like eating a balanced diet, staying active, and reducing stress can improve insulin sensitivity. Speak to your doctor for advice and use tools like continuous glucose monitors to track your progress. Taking control of your health now can help prevent serious complications in the future.
The Vively app can offer invaluable support in this process. It helps users monitor their glucose levels using CGM sensors, offers personalised health recommendations, and provides the necessary tools to lead a healthier lifestyle. With Vively, you can actively work towards better glucose control, reducing the risk of insulin resistance and its associated conditions.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Delve into an informative guide to understanding insulin resistance – its causes, signs and symptoms, testing methods, and how to effectively prevent it.
The term insulin resistance, also known as impaired insulin sensitivity, is often associated with prediabetes and type 2 diabetes. However, anyone can develop it, particularly if they lead a sedentary lifestyle or do not maintain a balanced diet. Even individuals without diabetes can experience this condition. If not managed effectively, impaired insulin sensitivity can progress to type 2 diabetes.
Insulin plays an essential role in your body's performance beyond regulating blood glucose levels. It allows blood sugar to enter cells for energy and tells the liver to store glucose for later use. It is necessary for the metabolism of carbohydrates, lipids, and proteins, which drives cell growth and provides the body with energy.
Impaired insulin sensitivity means that your body isn't utilising insulin effectively. This inefficiency requires a higher level of insulin to deliver glucose to fat and muscle cells.
The pancreas attempts to compensate by producing more insulin, to allow the glucose to enter the cells. However, the pancreatic cells that produce insulin can quickly deteriorate. When this happens, high blood sugar levels occur, increasing your risk for type 2 diabetes or prediabetes.
It can also lead to metabolic syndrome, heightening the risk of heart disease, kidney disease, obesity, polycystic ovary syndrome (PCOS), non-alcoholic fatty liver disease, among other conditions.
Insulin resistance symptoms may not be apparent in some people because their pancreas can still increase the body's insulin level to avoid excessive glucose in the bloodstream. However, with more significant insulin resistance, individuals may experience symptoms such as:
If you are experiencing these symptoms or are concerned, please speak with your healthcare professional.
To diagnose insulin resistance, healthcare professionals evaluate various aspects of a patient's health, including:
In terms of testing, the tests generally assess your blood glucose levels. Some of the most common insulin resistance tests in Australia include:

Keep in mind that the normal levels for these tests may vary. It's important to seek the guidance of your doctor for interpreting your test results.
Some individuals may also be asked to do a blood test to assess their lipids. These blood tests often measure triglycerides, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and total cholesterol. People with insulin resistance often have high triglyceride and low HDL levels as well as high levels of blood sugar.
The primary objective when managing insulin resistance is to restore your body's sensitivity to insulin, and stabilise your glucose levels so that cells can efficiently absorb glucose. Several lifestyle adjustments can help improve insulin sensitivity and reverse insulin resistance:
Some individuals may require medication to help manage their blood sugar. Discuss options with your doctor to determine a suitable insulin resistance management plan.
Continuous glucose monitoring (CGM) helps track blood sugar levels in real time. It provides valuable insights into how food, exercise, and daily habits affect glucose levels. For those managing insulin resistance, CGM can make a big difference in understanding patterns and making better decisions.
A small sensor placed under the skin measures glucose levels throughout the day. The data is sent to a device or smartphone app, showing trends and spikes in real time. This helps identify how meals or activities impact blood sugar.
Regularly reviewing CGM data with a doctor or dietitian can help create a tailored plan. Adjustments to meals, exercise, or medication can improve insulin sensitivity. Over time, these changes may lower the risk of type 2 diabetes.
Adding CGM to your health routine makes managing insulin resistance easier. It provides continuous feedback, making it a helpful tool for long-term success.
Early action is key to managing insulin resistance and reducing the risk of type 2 diabetes. Understanding its causes, symptoms, and testing options helps in making informed choices. Simple steps like eating a balanced diet, staying active, and reducing stress can improve insulin sensitivity. Speak to your doctor for advice and use tools like continuous glucose monitors to track your progress. Taking control of your health now can help prevent serious complications in the future.
The Vively app can offer invaluable support in this process. It helps users monitor their glucose levels using CGM sensors, offers personalised health recommendations, and provides the necessary tools to lead a healthier lifestyle. With Vively, you can actively work towards better glucose control, reducing the risk of insulin resistance and its associated conditions.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
