Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan



Your smartwatch buzzes gently as you prepare for bed, displaying a number that might seem unremarkable: your resting heart rate. But what if this simple metric could unlock profound insights into your sleep quality, metabolic health, and overall wellbeing?
Recent research reveals that your resting heart rate before bed isn't just another data point – it's a powerful window into your body's readiness for restorative sleep and metabolic recovery.
Understanding your normal resting heart rate before bed can transform how you approach sleep optimisation, helping you identify patterns that either support or sabotage your metabolic health goals.
Let's explore why this overlooked metric deserves a prominent place in your nightly routine.
Before diving into optimisation strategies, it's essential to understand what we're actually measuring and why this particular timing matters so much for your health.
Your resting heart rate represents the number of times your heart beats per minute when you're completely relaxed and at rest. While most people are familiar with daytime resting heart rate measurements, the pre-sleep reading offers unique insights into your body's preparation for the night ahead.
In most adults, resting heart rates range between 60 and 100 beats per minute during waking hours. However, your heart rate naturally begins to decline as bedtime approaches, reflecting your body's shift toward parasympathetic nervous system dominance – the "rest and digest" mode that promotes recovery and restoration.
The significance of monitoring your resting heart rate before bed extends far beyond simple curiosity. This metric serves as a real-time indicator of several critical physiological processes:
Autonomic nervous system balance: Your pre-sleep heart rate reflects the delicate balance between your sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) nervous systems. An elevated heart rate before bed often indicates that your sympathetic system remains overly active, potentially disrupting sleep quality and metabolic function.
Circadian rhythm alignment: Your heart rate naturally follows a circadian pattern, with lower rates typically occurring in the evening and during sleep. Disruptions to this pattern can signal misalignment between your internal body clock and your actual sleep schedule.
Metabolic readiness: Research demonstrates fascinating connections between heart rate patterns and metabolic processes. Studies have revealed moderate correlations between heart rate variations and glucose fluctuations during sleep, indicating that glucose fluctuations can be detected through heart rate monitoring.
Now that we understand what makes pre-sleep heart rate unique, let's explore the fascinating research that reveals why this timing is so critical for metabolic health.
Recent scientific investigations have illuminated the intricate relationship between sleep timing, heart rate regulation, and metabolic health. Research published in npj Digital Medicine found that deviations from normal bedtimes are associated with short-term increases in resting heart rate, highlighting the importance of bedtime regularity for cardiovascular health.
This finding challenges the common assumption that sleep duration alone determines sleep quality. Instead, consistency in sleep timing appears crucial for maintaining optimal cardiovascular and metabolic function.
Understanding these scientific mechanisms provides the foundation for interpreting your own readings. The physiological processes underlying these connections involve complex interactions between your circadian clock, autonomic nervous system, and metabolic processes.
During normal sleep preparation, your body initiates a cascade of changes:
Heart rate variability optimisation
As you prepare for sleep, your heart rate variability (HRV) – the variation in time between heartbeats – typically increases. This reflects enhanced parasympathetic activity and improved autonomic flexibility. Research examining the relationship between sleep duration and quality with heart rate variability has shown significant associations with cardiovascular health markers.
Metabolic hormone regulation
The evening hours trigger important hormonal shifts that influence both sleep quality and metabolic function. Cortisol levels naturally decline, while growth hormone production increases in preparation for overnight tissue repair and metabolic regulation.
Glucose regulation patterns
Studies using continuous glucose monitoring during sleep have revealed dynamic nocturnal glucose changes that correlate with heart rate patterns, particularly in response to sympathetic activation and sleep fragmentation. This connection suggests that monitoring heart rate before bed could provide insights into overnight glucose stability.
Want to see how strength training fits into your metabolic goals? Read our post on how bicep exercises improve your metabolic health.
With this scientific foundation in place, let's turn to the practical aspects of measurement and interpretation that you can implement tonight.
Accurately measuring your resting heart rate before bed requires consistent technique and timing. The most reliable approach involves taking measurements at the same time each evening, ideally 30-60 minutes before your intended sleep time, when you're relaxed but not yet drowsy.
Measurement techniques
Understanding how to measure your resting heart rate is just the beginning. Next, let’s explore what your numbers actually mean and how they reflect your metabolic health.
Once you've established your measurement routine, understanding what constitutes a normal reading becomes crucial. However, it's important to recognise that heart rate ranges vary significantly based on individual factors. The following table provides general guidelines for expected pre-sleep heart rates:

Note: These ranges represent pre-sleep heart rates, which are typically 20-30% lower than daytime resting rates. Individual variation is significant, and establishing your personal baseline is more important than comparing to population averages.
is more important than comparing to population averages.
Individual variation factors
While these ranges provide helpful guidance, your personal baseline can be influenced by numerous factors that extend beyond age and fitness level:
To fully appreciate what your pre-sleep reading means, it's helpful to understand how your heart rate evolves throughout the entire night.
Understanding how your heart rate changes during different sleep stages provides valuable context for interpreting your pre-sleep readings. Research shows distinct patterns that correlate with sleep quality and metabolic function.

Research demonstrates that sleep onset and progression to deeper sleep stages is associated with a shift toward greater parasympathetic modulation, whereas REM sleep is associated with greater sympathetic modulation. This explains why some people experience heart rate fluctuations during the night, particularly during REM cycles.
Interpreting patterns and trends
Armed with this knowledge of normal patterns, you can now interpret what your readings might be telling you about your health. Rather than focusing solely on absolute numbers, pay attention to patterns and deviations from your personal baseline. Here's what different patterns might indicate:
Consistently elevated pre-sleep heart rates (10+ bpm above baseline):
Significantly lower readings (15+ bpm below baseline):
High variability (daily fluctuations >15 bpm):
Now that you understand how to measure and interpret your readings, let's explore evidence-based strategies to optimise your pre-sleep heart rate for better metabolic health.
Achieving an optimal resting heart rate before bed requires a holistic approach that addresses both immediate evening practices and broader lifestyle factors. The following evidence-based strategies can help you create conditions for natural heart rate reduction and improved sleep preparation.
Research suggests that effective sleep preparation begins approximately 90 minutes before bedtime, aligning with your natural circadian rhythm decline. This protocol systematically prepares your body for sleep through targeted interventions:
Phase 1: Preparation (90-60 minutes before bed)
Phase 2: Transition (60-30 minutes before bed)
Phase 3: Final preparation (30-0 minutes before bed)
Building on the foundation of proper timing, specific relaxation techniques can provide measurable heart rate reductions. Different relaxation methods produce varying degrees of heart rate reduction.
The following table summarises techniques with their expected impact and time requirements:

Deep breathing protocols
Among the techniques listed above, deep breathing exercises offer the most immediate and accessible benefits. The 4-7-8 technique offers immediate heart rate benefits and can be performed anywhere. Inhale quietly through your nose for 4 counts, hold your breath for 7 counts, then exhale completely through your mouth for 8 counts. Repeat this cycle 3-4 times initially, gradually building to 8 cycles as you become more comfortable.
Box breathing provides similar benefits with a simpler pattern. Inhale for 4 counts, hold for 4, exhale for 4, and hold empty for 4. This technique is particularly effective for individuals who find breath-holding challenging.
Beyond personal techniques, your physical environment plays a crucial role in supporting natural heart rate reduction. Your sleep environment significantly influences your pre-sleep heart rate through multiple physiological pathways. Creating optimal conditions supports natural heart rate decline and improved sleep quality.
Temperature management
Your body naturally reduces core temperature in preparation for sleep, and supporting this process facilitates heart rate reduction. The optimal bedroom temperature ranges between 15-19°C (60-67°F), though individual preferences vary within this range.
Consider taking a warm bath or shower 1-2 hours before bedtime. This initially raises body temperature but triggers a subsequent cooling response that promotes sleepiness and heart rate reduction. The contrast between warm water and cooler air temperature enhances this thermoregulatory response.
Light exposure control
Exposure to bright light, particularly blue light from electronic devices, can suppress melatonin production and maintain elevated heart rates. Implement a "digital sunset" by dimming lights and switching devices to night mode 2-3 hours before bed.
Use warm, dim lighting (2700K or lower colour temperature) in the evening. Red or amber lighting has minimal impact on circadian rhythms and may actually support heart rate reduction.
Sound environment
Sudden noises can cause heart rate spikes even during light sleep stages. Create a consistent sound environment using white noise, earplugs, or sound-masking techniques. If you use background sounds, choose consistent, non-varying options like steady rainfall or ocean waves rather than music with changing rhythms and melodies.
Complementing environmental optimisation, what and when you eat significantly impacts your pre-sleep heart rate. The timing and composition of your evening food and drink intake directly influence your pre-sleep heart rate through metabolic and thermic effects.
Complete your last substantial meal 3-4 hours before bedtime to allow adequate digestion. Large meals require significant metabolic energy and can maintain elevated heart rates for 2-4 hours post-consumption.
If you need to eat within 2 hours of bedtime, choose easily digestible options under 200 calories. Focus on foods with a higher protein-to-carbohydrate ratio to minimise glucose fluctuations that can affect heart rate stability.
For more on why building metabolic fitness matters for long-term health, check out our guide on why metabolic fitness is important.
Certain foods contain compounds that may support heart rate reduction and sleep quality:
Substance considerations
Caffeine sensitivity varies dramatically among individuals, with half-life ranging from 3-7 hours. Monitor how afternoon and evening caffeine intake correlates with your pre-sleep heart rate measurements. Some individuals need to avoid caffeine after 12 PM to achieve optimal pre-sleep heart rates.
Alcohol presents complex effects on heart rate and sleep. While it may initially seem relaxing and cause a temporary heart rate reduction, alcohol disrupts sleep architecture and often causes heart rate fluctuations throughout the night, particularly during REM sleep phases.
Leg workouts do more than build strength. They play a major role in supporting metabolic health. Learn more in our blog on how leg exercises improve your metabolism.
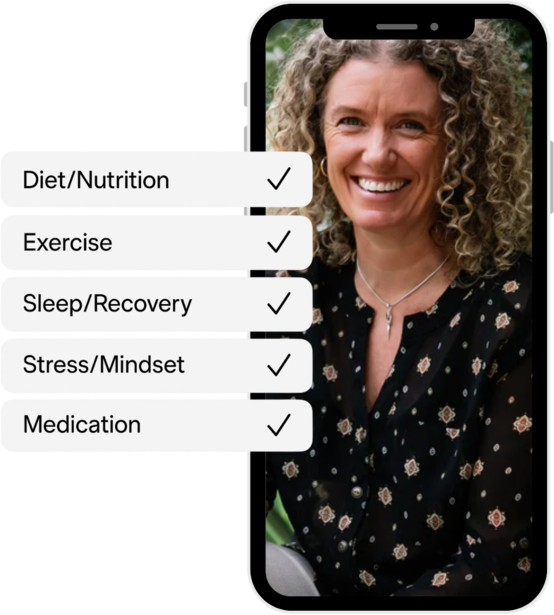
At Vively, we know that optimal metabolic health comes from understanding how your body responds to daily habits—across sleep, stress, nutrition, and activity. That’s why we created the Metabolic Health Score, a simple yet powerful way to track your overall metabolic function based on real-time data.

This score is generated using key glucose measures such as average glucose, glucose variability, time in range, fasting glucose, and estimated HbA1c. It gives you a clear picture of how well your metabolism is functioning and highlights where improvements can be made.
Our CGM technology continuously monitors your glucose levels, giving you real-time feedback on how your meals, workouts, sleep, and stress are affecting your score. You can also log other health markers like heart rate, sleep quality, and mood directly in the Vively app—connecting all aspects of your lifestyle in one place.
With support from our qualified health coaches, you’ll get guidance on how to improve your Metabolic Health Score over time. This includes personalised recommendations for your diet, exercise, stress management, and sleep routine—based on your own data trends.
Every insight and action plan you receive is tailored to your metabolic data, not general assumptions. Whether you’re looking to reduce glucose spikes, improve overnight recovery, or stabilise your energy levels, your score provides a clear starting point.
Track your score, understand your patterns, and get expert guidance with the Vively app—your personal tool for long-term metabolic wellbeing.
As you begin implementing these strategies, you'll likely have questions about what's normal, what to expect, and when to seek additional support. Here are the most common questions we encounter:
A normal sleeping heart rate typically runs about 20% to 30% lower than your daytime resting heart rate. For most adults, this means a pre-sleep heart rate between 45-70 beats per minute, though individual variation is significant based on age, fitness level, and other factors. Athletes and highly fit individuals may see pre-sleep rates as low as 40-50 bpm, while sedentary adults might range from 55-75 bpm.
An elevated resting heart rate before bed often indicates sympathetic nervous system activation, which can interfere with your body's natural transition to sleep. Research shows that sleep onset and progression to deeper sleep stages is associated with a shift toward greater parasympathetic modulation, whereas REM sleep is associated with greater sympathetic modulation.
Higher pre-sleep heart rates are associated with longer sleep onset times, more fragmented sleep, and reduced overall sleep quality.
Yes, monitoring your pre-sleep heart rate can provide insights into stress levels, sleep quality, and circadian rhythm alignment – all factors that significantly influence metabolic health and weight management.
Generally low resting heart rate and high heart rate variability are good indicators of sufficient recovery, which supports optimal metabolic function. Poor sleep quality, indicated by consistently elevated pre-sleep heart rates, is associated with increased cortisol production, disrupted hunger hormones, and impaired glucose regulation.
Several factors can elevate your pre-sleep heart rate, including: late caffeine consumption (effects can persist 6-8 hours), large meals close to bedtime (metabolic demands increase heart rate for 2-4 hours), stress or anxiety, room temperature above 22°C, recent intense exercise (within 3-4 hours), certain medications (stimulants, decongestants), dehydration, or underlying health conditions.
Environmental factors like noise, bright light exposure, or uncomfortable bedding can also maintain elevated readings.
Some variation is normal, but consistently high readings or sudden significant changes warrant attention.
Daily variations of 5-10 bpm are typical, but variations exceeding 15 bpm or sustained elevations above your baseline may indicate: sleep disorders, chronic stress, overtraining (in athletes), medication effects, illness or infection, or cardiovascular issues.
Track patterns over time rather than focusing on individual readings. If you notice persistent elevation (>2 weeks) or concerning changes, consult with a healthcare provider to rule out underlying issues.
Timeline for improvements varies based on the interventions implemented: immediate changes (1-7 days) can result from eliminating late caffeine, improving sleep environment temperature, or implementing breathing exercises.
Short-term changes (1-4 weeks) may come from consistent sleep timing, dietary modifications, and stress management techniques. Long-term improvements (1-3 months) typically result from sustained lifestyle changes, improved fitness levels, and chronic stress reduction.
Heart rate variability shows you how well your body is recovered, if you're overtraining, and if you need to improve how you handle stress, making it an excellent metric for tracking progress over time.
Research demonstrates fascinating connections between heart rate patterns and metabolic processes during sleep. Studies have revealed correlations between heart rate variations and glucose fluctuations during sleep, indicating that glucose changes can be detected through heart rate monitoring.
Elevated pre-sleep heart rates may indicate sympathetic nervous system activation, which can affect overnight glucose regulation through increased cortisol and decreased insulin sensitivity. This connection makes pre-sleep heart rate monitoring particularly valuable for individuals managing diabetes or metabolic syndrome.
Throughout this guide, we've seen how a simple number—your resting heart rate before bed—can reveal a lot about your sleep quality and metabolic health.
At Vively, we make it easier to track this important metric alongside your glucose data, helping you see how your body responds to daily habits like meals, exercise, and stress. With personalised insights and coaching, you don’t have to figure it all out alone. Vively helps you understand your unique patterns and gives you the tools to make smarter decisions for your health.
Your resting heart rate is more than just a number—it’s a signal. Use it to shape a more supportive evening routine, improve recovery overnight, and strengthen your metabolic health over time.
Want support as you start tracking your heart rate and glucose together? Join Vively today and take control of your metabolic wellbeing.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Your smartwatch buzzes gently as you prepare for bed, displaying a number that might seem unremarkable: your resting heart rate. But what if this simple metric could unlock profound insights into your sleep quality, metabolic health, and overall wellbeing?
Recent research reveals that your resting heart rate before bed isn't just another data point – it's a powerful window into your body's readiness for restorative sleep and metabolic recovery.
Understanding your normal resting heart rate before bed can transform how you approach sleep optimisation, helping you identify patterns that either support or sabotage your metabolic health goals.
Let's explore why this overlooked metric deserves a prominent place in your nightly routine.
Before diving into optimisation strategies, it's essential to understand what we're actually measuring and why this particular timing matters so much for your health.
Your resting heart rate represents the number of times your heart beats per minute when you're completely relaxed and at rest. While most people are familiar with daytime resting heart rate measurements, the pre-sleep reading offers unique insights into your body's preparation for the night ahead.
In most adults, resting heart rates range between 60 and 100 beats per minute during waking hours. However, your heart rate naturally begins to decline as bedtime approaches, reflecting your body's shift toward parasympathetic nervous system dominance – the "rest and digest" mode that promotes recovery and restoration.
The significance of monitoring your resting heart rate before bed extends far beyond simple curiosity. This metric serves as a real-time indicator of several critical physiological processes:
Autonomic nervous system balance: Your pre-sleep heart rate reflects the delicate balance between your sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) nervous systems. An elevated heart rate before bed often indicates that your sympathetic system remains overly active, potentially disrupting sleep quality and metabolic function.
Circadian rhythm alignment: Your heart rate naturally follows a circadian pattern, with lower rates typically occurring in the evening and during sleep. Disruptions to this pattern can signal misalignment between your internal body clock and your actual sleep schedule.
Metabolic readiness: Research demonstrates fascinating connections between heart rate patterns and metabolic processes. Studies have revealed moderate correlations between heart rate variations and glucose fluctuations during sleep, indicating that glucose fluctuations can be detected through heart rate monitoring.
Now that we understand what makes pre-sleep heart rate unique, let's explore the fascinating research that reveals why this timing is so critical for metabolic health.
Recent scientific investigations have illuminated the intricate relationship between sleep timing, heart rate regulation, and metabolic health. Research published in npj Digital Medicine found that deviations from normal bedtimes are associated with short-term increases in resting heart rate, highlighting the importance of bedtime regularity for cardiovascular health.
This finding challenges the common assumption that sleep duration alone determines sleep quality. Instead, consistency in sleep timing appears crucial for maintaining optimal cardiovascular and metabolic function.
Understanding these scientific mechanisms provides the foundation for interpreting your own readings. The physiological processes underlying these connections involve complex interactions between your circadian clock, autonomic nervous system, and metabolic processes.
During normal sleep preparation, your body initiates a cascade of changes:
Heart rate variability optimisation
As you prepare for sleep, your heart rate variability (HRV) – the variation in time between heartbeats – typically increases. This reflects enhanced parasympathetic activity and improved autonomic flexibility. Research examining the relationship between sleep duration and quality with heart rate variability has shown significant associations with cardiovascular health markers.
Metabolic hormone regulation
The evening hours trigger important hormonal shifts that influence both sleep quality and metabolic function. Cortisol levels naturally decline, while growth hormone production increases in preparation for overnight tissue repair and metabolic regulation.
Glucose regulation patterns
Studies using continuous glucose monitoring during sleep have revealed dynamic nocturnal glucose changes that correlate with heart rate patterns, particularly in response to sympathetic activation and sleep fragmentation. This connection suggests that monitoring heart rate before bed could provide insights into overnight glucose stability.
Want to see how strength training fits into your metabolic goals? Read our post on how bicep exercises improve your metabolic health.
With this scientific foundation in place, let's turn to the practical aspects of measurement and interpretation that you can implement tonight.
Accurately measuring your resting heart rate before bed requires consistent technique and timing. The most reliable approach involves taking measurements at the same time each evening, ideally 30-60 minutes before your intended sleep time, when you're relaxed but not yet drowsy.
Measurement techniques
Understanding how to measure your resting heart rate is just the beginning. Next, let’s explore what your numbers actually mean and how they reflect your metabolic health.
Once you've established your measurement routine, understanding what constitutes a normal reading becomes crucial. However, it's important to recognise that heart rate ranges vary significantly based on individual factors. The following table provides general guidelines for expected pre-sleep heart rates:

Note: These ranges represent pre-sleep heart rates, which are typically 20-30% lower than daytime resting rates. Individual variation is significant, and establishing your personal baseline is more important than comparing to population averages.
is more important than comparing to population averages.
Individual variation factors
While these ranges provide helpful guidance, your personal baseline can be influenced by numerous factors that extend beyond age and fitness level:
To fully appreciate what your pre-sleep reading means, it's helpful to understand how your heart rate evolves throughout the entire night.
Understanding how your heart rate changes during different sleep stages provides valuable context for interpreting your pre-sleep readings. Research shows distinct patterns that correlate with sleep quality and metabolic function.

Research demonstrates that sleep onset and progression to deeper sleep stages is associated with a shift toward greater parasympathetic modulation, whereas REM sleep is associated with greater sympathetic modulation. This explains why some people experience heart rate fluctuations during the night, particularly during REM cycles.
Interpreting patterns and trends
Armed with this knowledge of normal patterns, you can now interpret what your readings might be telling you about your health. Rather than focusing solely on absolute numbers, pay attention to patterns and deviations from your personal baseline. Here's what different patterns might indicate:
Consistently elevated pre-sleep heart rates (10+ bpm above baseline):
Significantly lower readings (15+ bpm below baseline):
High variability (daily fluctuations >15 bpm):
Now that you understand how to measure and interpret your readings, let's explore evidence-based strategies to optimise your pre-sleep heart rate for better metabolic health.
Achieving an optimal resting heart rate before bed requires a holistic approach that addresses both immediate evening practices and broader lifestyle factors. The following evidence-based strategies can help you create conditions for natural heart rate reduction and improved sleep preparation.
Research suggests that effective sleep preparation begins approximately 90 minutes before bedtime, aligning with your natural circadian rhythm decline. This protocol systematically prepares your body for sleep through targeted interventions:
Phase 1: Preparation (90-60 minutes before bed)
Phase 2: Transition (60-30 minutes before bed)
Phase 3: Final preparation (30-0 minutes before bed)
Building on the foundation of proper timing, specific relaxation techniques can provide measurable heart rate reductions. Different relaxation methods produce varying degrees of heart rate reduction.
The following table summarises techniques with their expected impact and time requirements:

Deep breathing protocols
Among the techniques listed above, deep breathing exercises offer the most immediate and accessible benefits. The 4-7-8 technique offers immediate heart rate benefits and can be performed anywhere. Inhale quietly through your nose for 4 counts, hold your breath for 7 counts, then exhale completely through your mouth for 8 counts. Repeat this cycle 3-4 times initially, gradually building to 8 cycles as you become more comfortable.
Box breathing provides similar benefits with a simpler pattern. Inhale for 4 counts, hold for 4, exhale for 4, and hold empty for 4. This technique is particularly effective for individuals who find breath-holding challenging.
Beyond personal techniques, your physical environment plays a crucial role in supporting natural heart rate reduction. Your sleep environment significantly influences your pre-sleep heart rate through multiple physiological pathways. Creating optimal conditions supports natural heart rate decline and improved sleep quality.
Temperature management
Your body naturally reduces core temperature in preparation for sleep, and supporting this process facilitates heart rate reduction. The optimal bedroom temperature ranges between 15-19°C (60-67°F), though individual preferences vary within this range.
Consider taking a warm bath or shower 1-2 hours before bedtime. This initially raises body temperature but triggers a subsequent cooling response that promotes sleepiness and heart rate reduction. The contrast between warm water and cooler air temperature enhances this thermoregulatory response.
Light exposure control
Exposure to bright light, particularly blue light from electronic devices, can suppress melatonin production and maintain elevated heart rates. Implement a "digital sunset" by dimming lights and switching devices to night mode 2-3 hours before bed.
Use warm, dim lighting (2700K or lower colour temperature) in the evening. Red or amber lighting has minimal impact on circadian rhythms and may actually support heart rate reduction.
Sound environment
Sudden noises can cause heart rate spikes even during light sleep stages. Create a consistent sound environment using white noise, earplugs, or sound-masking techniques. If you use background sounds, choose consistent, non-varying options like steady rainfall or ocean waves rather than music with changing rhythms and melodies.
Complementing environmental optimisation, what and when you eat significantly impacts your pre-sleep heart rate. The timing and composition of your evening food and drink intake directly influence your pre-sleep heart rate through metabolic and thermic effects.
Complete your last substantial meal 3-4 hours before bedtime to allow adequate digestion. Large meals require significant metabolic energy and can maintain elevated heart rates for 2-4 hours post-consumption.
If you need to eat within 2 hours of bedtime, choose easily digestible options under 200 calories. Focus on foods with a higher protein-to-carbohydrate ratio to minimise glucose fluctuations that can affect heart rate stability.
For more on why building metabolic fitness matters for long-term health, check out our guide on why metabolic fitness is important.
Certain foods contain compounds that may support heart rate reduction and sleep quality:
Substance considerations
Caffeine sensitivity varies dramatically among individuals, with half-life ranging from 3-7 hours. Monitor how afternoon and evening caffeine intake correlates with your pre-sleep heart rate measurements. Some individuals need to avoid caffeine after 12 PM to achieve optimal pre-sleep heart rates.
Alcohol presents complex effects on heart rate and sleep. While it may initially seem relaxing and cause a temporary heart rate reduction, alcohol disrupts sleep architecture and often causes heart rate fluctuations throughout the night, particularly during REM sleep phases.
Leg workouts do more than build strength. They play a major role in supporting metabolic health. Learn more in our blog on how leg exercises improve your metabolism.
At Vively, we know that optimal metabolic health comes from understanding how your body responds to daily habits—across sleep, stress, nutrition, and activity. That’s why we created the Metabolic Health Score, a simple yet powerful way to track your overall metabolic function based on real-time data.

This score is generated using key glucose measures such as average glucose, glucose variability, time in range, fasting glucose, and estimated HbA1c. It gives you a clear picture of how well your metabolism is functioning and highlights where improvements can be made.
Our CGM technology continuously monitors your glucose levels, giving you real-time feedback on how your meals, workouts, sleep, and stress are affecting your score. You can also log other health markers like heart rate, sleep quality, and mood directly in the Vively app—connecting all aspects of your lifestyle in one place.
With support from our qualified health coaches, you’ll get guidance on how to improve your Metabolic Health Score over time. This includes personalised recommendations for your diet, exercise, stress management, and sleep routine—based on your own data trends.
Every insight and action plan you receive is tailored to your metabolic data, not general assumptions. Whether you’re looking to reduce glucose spikes, improve overnight recovery, or stabilise your energy levels, your score provides a clear starting point.
Track your score, understand your patterns, and get expert guidance with the Vively app—your personal tool for long-term metabolic wellbeing.
As you begin implementing these strategies, you'll likely have questions about what's normal, what to expect, and when to seek additional support. Here are the most common questions we encounter:
A normal sleeping heart rate typically runs about 20% to 30% lower than your daytime resting heart rate. For most adults, this means a pre-sleep heart rate between 45-70 beats per minute, though individual variation is significant based on age, fitness level, and other factors. Athletes and highly fit individuals may see pre-sleep rates as low as 40-50 bpm, while sedentary adults might range from 55-75 bpm.
An elevated resting heart rate before bed often indicates sympathetic nervous system activation, which can interfere with your body's natural transition to sleep. Research shows that sleep onset and progression to deeper sleep stages is associated with a shift toward greater parasympathetic modulation, whereas REM sleep is associated with greater sympathetic modulation.
Higher pre-sleep heart rates are associated with longer sleep onset times, more fragmented sleep, and reduced overall sleep quality.
Yes, monitoring your pre-sleep heart rate can provide insights into stress levels, sleep quality, and circadian rhythm alignment – all factors that significantly influence metabolic health and weight management.
Generally low resting heart rate and high heart rate variability are good indicators of sufficient recovery, which supports optimal metabolic function. Poor sleep quality, indicated by consistently elevated pre-sleep heart rates, is associated with increased cortisol production, disrupted hunger hormones, and impaired glucose regulation.
Several factors can elevate your pre-sleep heart rate, including: late caffeine consumption (effects can persist 6-8 hours), large meals close to bedtime (metabolic demands increase heart rate for 2-4 hours), stress or anxiety, room temperature above 22°C, recent intense exercise (within 3-4 hours), certain medications (stimulants, decongestants), dehydration, or underlying health conditions.
Environmental factors like noise, bright light exposure, or uncomfortable bedding can also maintain elevated readings.
Some variation is normal, but consistently high readings or sudden significant changes warrant attention.
Daily variations of 5-10 bpm are typical, but variations exceeding 15 bpm or sustained elevations above your baseline may indicate: sleep disorders, chronic stress, overtraining (in athletes), medication effects, illness or infection, or cardiovascular issues.
Track patterns over time rather than focusing on individual readings. If you notice persistent elevation (>2 weeks) or concerning changes, consult with a healthcare provider to rule out underlying issues.
Timeline for improvements varies based on the interventions implemented: immediate changes (1-7 days) can result from eliminating late caffeine, improving sleep environment temperature, or implementing breathing exercises.
Short-term changes (1-4 weeks) may come from consistent sleep timing, dietary modifications, and stress management techniques. Long-term improvements (1-3 months) typically result from sustained lifestyle changes, improved fitness levels, and chronic stress reduction.
Heart rate variability shows you how well your body is recovered, if you're overtraining, and if you need to improve how you handle stress, making it an excellent metric for tracking progress over time.
Research demonstrates fascinating connections between heart rate patterns and metabolic processes during sleep. Studies have revealed correlations between heart rate variations and glucose fluctuations during sleep, indicating that glucose changes can be detected through heart rate monitoring.
Elevated pre-sleep heart rates may indicate sympathetic nervous system activation, which can affect overnight glucose regulation through increased cortisol and decreased insulin sensitivity. This connection makes pre-sleep heart rate monitoring particularly valuable for individuals managing diabetes or metabolic syndrome.
Throughout this guide, we've seen how a simple number—your resting heart rate before bed—can reveal a lot about your sleep quality and metabolic health.
At Vively, we make it easier to track this important metric alongside your glucose data, helping you see how your body responds to daily habits like meals, exercise, and stress. With personalised insights and coaching, you don’t have to figure it all out alone. Vively helps you understand your unique patterns and gives you the tools to make smarter decisions for your health.
Your resting heart rate is more than just a number—it’s a signal. Use it to shape a more supportive evening routine, improve recovery overnight, and strengthen your metabolic health over time.
Want support as you start tracking your heart rate and glucose together? Join Vively today and take control of your metabolic wellbeing.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
