Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan



If you’ve been searching for Function Health, you’re probably looking for something more advanced than a basic blood test. Function has become known for large biomarker panels, longevity-focused testing, and digital health insights.
Here’s the key thing to know straight away:
Function Health is not available in Australia.
But if your goal is the same — a comprehensive, whole-body view of your health with real guidance on what to do next — there is a comparable option locally. The approach just looks a little different.
Function Health is a US-based subscription service built around extensive blood testing. Members complete:
The focus is wide screening across cardiovascular risk, metabolic health, hormones, inflammation, nutrients, liver, kidney and more. It’s designed for people who want deeper insight than a routine GP panel.
In simple terms: lots of data, organised in one place.
Most people drawn to Function Health are trying to be proactive. They want:
This reflects a growing shift toward preventive and metabolic health testing rather than waiting for symptoms.
Function Health currently operates in the United States only. Australians can’t sign up.
There’s also a structural difference worth understanding. Function is primarily a large lab testing platform. It provides a comprehensive snapshot and written commentary, but ongoing lifestyle coaching, real-time metabolic feedback, and day-to-day tracking aren’t central parts of the model.
That’s where the closest Australian alternative takes a different approach.
For Australians searching “Function Health Australia” or “a test like Function Health,” Vively’s Full Body Health Check and metabolic health program is the closest local equivalent.
It combines broad biomarker testing with clinical interpretation and ongoing support to help you act on the data.
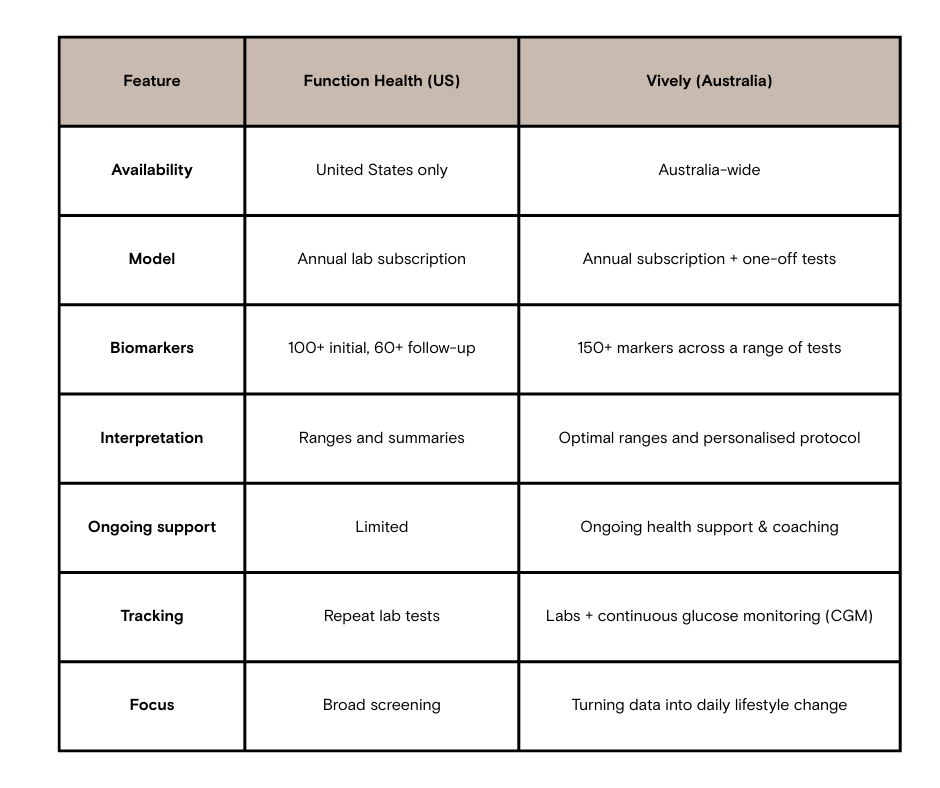
Both approaches aim to give a deeper understanding of your health. The difference is what happens after the blood draw.
Function Health excels at delivering a large volume of lab data in a structured way. For people who want extensive screening, that can be valuable.
Vively is built around a different idea:
Blood tests show what’s happening. Daily data shows why.
With Vively:
It’s designed as an ongoing metabolic health system, rather than a periodic screening event.
More data can be useful, but interpretation matters. Large panels often include markers that fluctuate or need context. Without structured follow-up, people can end up with information but no clear plan.
That’s why integrated clinical review and lifestyle guidance become important alongside advanced testing.
Function Health may suit you if:
Vively suits Australians who want:
Is Function Health available in Australia?
No, the service currently operates in the United States only.
What is the closest alternative to Function Health in Australia?
Programs that combine broad biomarker testing with GP interpretation and ongoing metabolic tracking, such as Vively’s Full Body Health Check and CGM-based support, provide a similar level of depth.
How many biomarkers should a comprehensive blood test include?
A full panel typically covers cardiovascular, metabolic, hormonal, liver, kidney, inflammatory and nutrient markers. The usefulness comes from interpretation and follow-through, not just the number.
Do advanced blood tests require clinical guidance?
Yes. Larger panels increase the need for context, prioritisation, and structured follow-up.
What’s the difference between a blood panel and metabolic tracking?
A blood panel shows internal markers at a point in time. Metabolic tracking, such as CGM, shows how daily behaviours affect physiology in real time.
Function Health represents a data-heavy, large-panel testing model, but it’s US-only.
For Australians looking for the same level of comprehensive insight, Vively’s Full Body Health Check and metabolic health program is the closest local alternative. The key difference isn’t just how many biomarkers are measured — it’s how effectively those results are turned into ongoing, actionable change that supports long-term health.
Subscribe to our newsletter & join a community of 20,000+ Aussies

If you’ve been searching for Function Health, you’re probably looking for something more advanced than a basic blood test. Function has become known for large biomarker panels, longevity-focused testing, and digital health insights.
Here’s the key thing to know straight away:
Function Health is not available in Australia.
But if your goal is the same — a comprehensive, whole-body view of your health with real guidance on what to do next — there is a comparable option locally. The approach just looks a little different.
Function Health is a US-based subscription service built around extensive blood testing. Members complete:
The focus is wide screening across cardiovascular risk, metabolic health, hormones, inflammation, nutrients, liver, kidney and more. It’s designed for people who want deeper insight than a routine GP panel.
In simple terms: lots of data, organised in one place.
Most people drawn to Function Health are trying to be proactive. They want:
This reflects a growing shift toward preventive and metabolic health testing rather than waiting for symptoms.
Function Health currently operates in the United States only. Australians can’t sign up.
There’s also a structural difference worth understanding. Function is primarily a large lab testing platform. It provides a comprehensive snapshot and written commentary, but ongoing lifestyle coaching, real-time metabolic feedback, and day-to-day tracking aren’t central parts of the model.
That’s where the closest Australian alternative takes a different approach.
For Australians searching “Function Health Australia” or “a test like Function Health,” Vively’s Full Body Health Check and metabolic health program is the closest local equivalent.
It combines broad biomarker testing with clinical interpretation and ongoing support to help you act on the data.
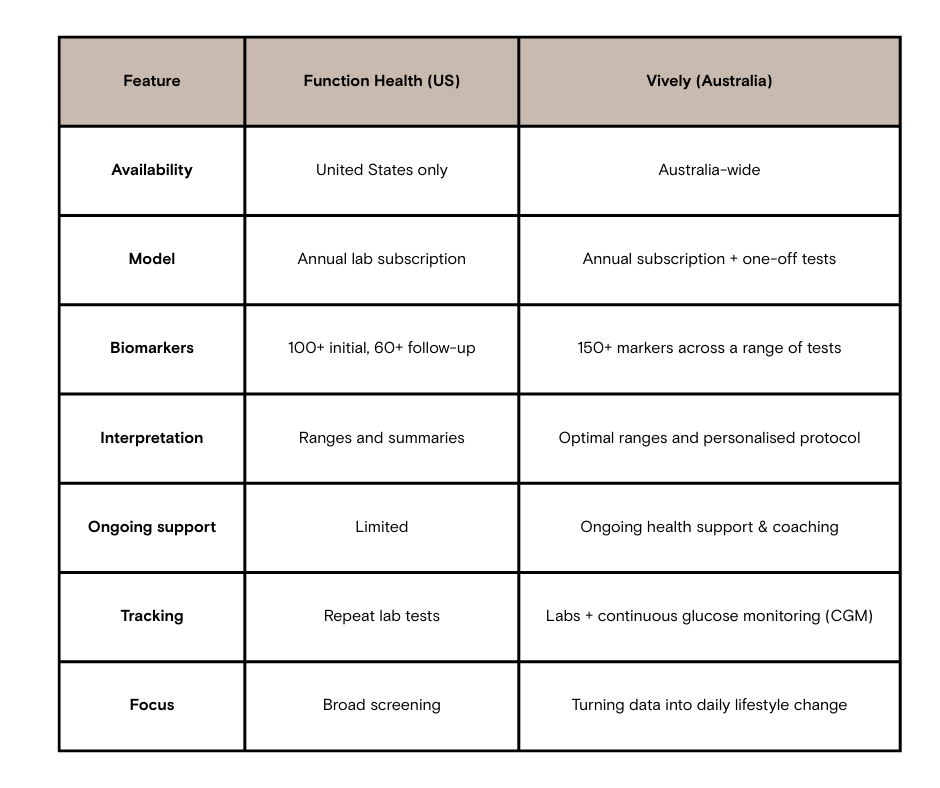
Both approaches aim to give a deeper understanding of your health. The difference is what happens after the blood draw.
Function Health excels at delivering a large volume of lab data in a structured way. For people who want extensive screening, that can be valuable.
Vively is built around a different idea:
Blood tests show what’s happening. Daily data shows why.
With Vively:
It’s designed as an ongoing metabolic health system, rather than a periodic screening event.
More data can be useful, but interpretation matters. Large panels often include markers that fluctuate or need context. Without structured follow-up, people can end up with information but no clear plan.
That’s why integrated clinical review and lifestyle guidance become important alongside advanced testing.
Function Health may suit you if:
Vively suits Australians who want:
Is Function Health available in Australia?
No, the service currently operates in the United States only.
What is the closest alternative to Function Health in Australia?
Programs that combine broad biomarker testing with GP interpretation and ongoing metabolic tracking, such as Vively’s Full Body Health Check and CGM-based support, provide a similar level of depth.
How many biomarkers should a comprehensive blood test include?
A full panel typically covers cardiovascular, metabolic, hormonal, liver, kidney, inflammatory and nutrient markers. The usefulness comes from interpretation and follow-through, not just the number.
Do advanced blood tests require clinical guidance?
Yes. Larger panels increase the need for context, prioritisation, and structured follow-up.
What’s the difference between a blood panel and metabolic tracking?
A blood panel shows internal markers at a point in time. Metabolic tracking, such as CGM, shows how daily behaviours affect physiology in real time.
Function Health represents a data-heavy, large-panel testing model, but it’s US-only.
For Australians looking for the same level of comprehensive insight, Vively’s Full Body Health Check and metabolic health program is the closest local alternative. The key difference isn’t just how many biomarkers are measured — it’s how effectively those results are turned into ongoing, actionable change that supports long-term health.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
