Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan




Want to stay healthier for longer? Testing key biomarkers can help you understand how your body is aging and identify areas to improve your healthspan. Here are five tests that provide actionable insights:
Fasting blood glucose (FBG) and HbA1c are two essential markers for understanding blood sugar control. They provide insights into both short-term and long-term glucose levels, which are crucial for maintaining overall health and longevity.
Keeping blood sugar levels in check plays a big role in healthy aging. Elevated blood sugar can significantly shorten healthspan. For instance, research shows that a one standard deviation increase in HbA1c is linked to a 29% higher chance of healthspan ending prematurely. On top of that, every 1% increase in HbA1c above 6% raises the risk of cardiovascular disease by 18%.
FBG provides a quick snapshot of blood sugar levels after fasting for 8–12 hours, while HbA1c reflects the average blood sugar levels over the past 2–3 months. Elevated HbA1c is not only a marker for diabetes but is also an independent risk factor for coronary heart disease and stroke.
Additionally, genetic tendencies toward higher fasting blood glucose are associated with a 5% increased risk of developing chronic diseases.
Both FBG and HbA1c tests are straightforward and widely available. FBG requires fasting for 8 to 12 hours before a blood draw, while HbA1c testing can be done at any time without fasting.
How often should you test?
Advanced tools like continuous glucose monitors (CGMs) provide real-time data, though they come with higher costs. Considering that over a third of U.S. adults have prediabetes, most without knowing it. CGMs can help uncover hidden blood sugar trends.
Healthy glucose levels are key to long-term wellbeing. An HbA1c level between 5.7% and 6.4% signals prediabetes, while a level of 6.5% or higher on two separate tests confirms diabetes. HbA1c is a more reliable indicator of long-term glucose control compared to fasting blood glucose, as it isn’t easily influenced by short-term factors like illness or stress.
Lifestyle changes can make a big difference in glucose management. Diet, exercise, and medical care all play a role in maintaining a healthy metabolic profile.
Some effective dietary tips include:
Physical activity and regular meal patterns also help regulate blood sugar levels.
For those using CGMs, these devices can integrate with sleep and stress data to predict glucose changes and provide alerts for timely intervention. When combined with stress management techniques and consistent monitoring, these strategies can significantly improve metabolic health and support a longer, healthier life.
Want to take your health tracking a step further? Check out our guide on improving blood markers naturally from CRP to HbA1c to see how small lifestyle changes add up.
A lipid panel measures four key markers: total cholesterol, LDL (low-density lipoprotein), HDL (high-density lipoprotein), and triglycerides. These numbers provide valuable insight into cardiovascular health and overall longevity.
An unhealthy lipid profile characterised by high LDL and triglycerides alongside low HDL is a significant risk factor for cardiovascular disease. Since heart disease is the leading cause of death in the United States, keeping these markers in check plays a critical role in maintaining a longer, healthier life.
High LDL levels are closely linked to atherosclerosis, which can lead to cardiovascular complications. Additionally, smaller LDL particle sizes are associated with higher risks of type 2 diabetes, metabolic syndrome, and coronary artery disease.
HDL, often called "good cholesterol", helps protect against heart disease by reducing inflammation and preventing LDL oxidation. On the other hand, elevated triglycerides are a hallmark of metabolic syndrome, which increases the likelihood of cardiovascular disease and type 2 diabetes. The triglyceride-to-HDL ratio is particularly telling; it’s a strong indicator of type 2 diabetes risk
Another useful metric is the total cholesterol to HDL ratio, which many studies suggest is a better predictor of heart disease than LDL alone. Ideally, this ratio should be 5:1 or lower, with 3.5:1 being the optimal target.
Regular lipid testing is straightforward, accessible, and affordable. It can be done at a doctor’s office, lab, clinic, or hospital, usually through a standard blood draw. Results are typically available quickly, making it easy to track changes over time.
Testing frequency depends on individual risk factors. Those with a family history of heart disease, diabetes, high blood pressure, or other risks such as smoking or obesity should monitor their levels more often. A healthcare provider can recommend an appropriate schedule based on your age and risk profile.
Cost isn’t a barrier for most people. Lipid panel tests at walk-in clinics or pharmacies often cost under $100. For added convenience, point-of-care testing using a finger prick or at-home kits offers quicker results, though these methods may not always provide the same level of accuracy as traditional lab tests.
Improving your lipid profile doesn’t require drastic measures. Consistent lifestyle changes can make a big difference.
By combining these strategies, you can support heart health and promote overall metabolic balance, key factors in extending your healthspan.
Research underscores the importance of lipid management in preventing chronic disease and promoting longevity. For instance, elevated Lp(a), a cholesterol particle linked to cardiovascular risk, affects approximately 1.5 billion people globally. With over 90% of Lp(a) levels determined by genetics, it’s the most common form of inherited dyslipidaemia.
Testing for Lp(a) is relatively affordable, ranging from $25 to $100, similar to standard lipid panels.
Regularly monitoring and optimising your lipid levels is a powerful way to reduce the risk of age-related chronic diseases and improve your long-term health outlook. By staying proactive, you can take meaningful steps toward a healthier, longer life.
Want to understand how hidden inflammation might be slowing you down? Read our article on chronic inflammation and the CRP blood test that reveals it.
High-sensitivity C-reactive protein (hs-CRP) is a test that measures even the smallest levels of inflammation in the body, offering more detailed insights compared to standard CRP tests. It serves as a reliable marker for chronic inflammation, which has been closely linked to aging and various chronic conditions.
Chronic inflammation, often termed "inflammaging", plays a key role in the aging process and contributes to the onset of age-related diseases. CRP is produced by the liver in response to inflammation, infections, or tissue damage. Research shows that hs-CRP levels above 3 mg/L can reduce life expectancy by up to 4 years, while keeping levels below 1 mg/L may extend lifespan by 8–10 years. Elevated hs-CRP levels are also strongly associated with a higher risk of cardiovascular disease and shorter lifespans.
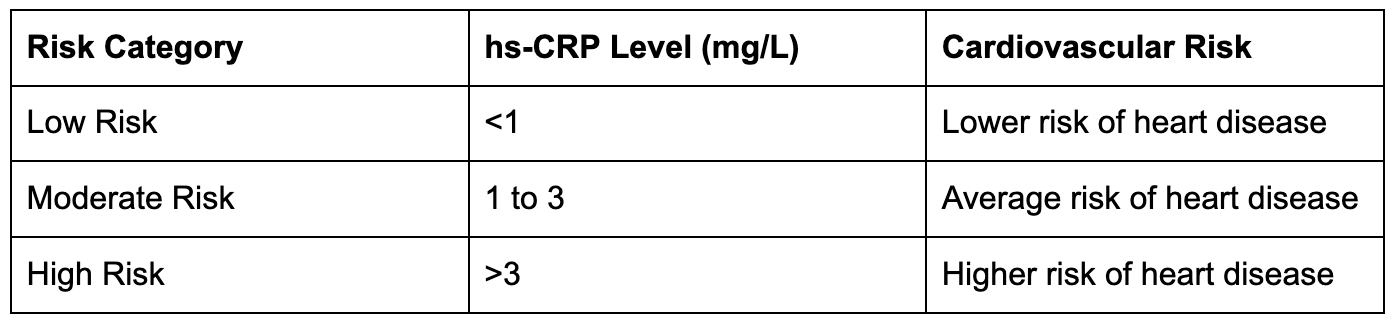
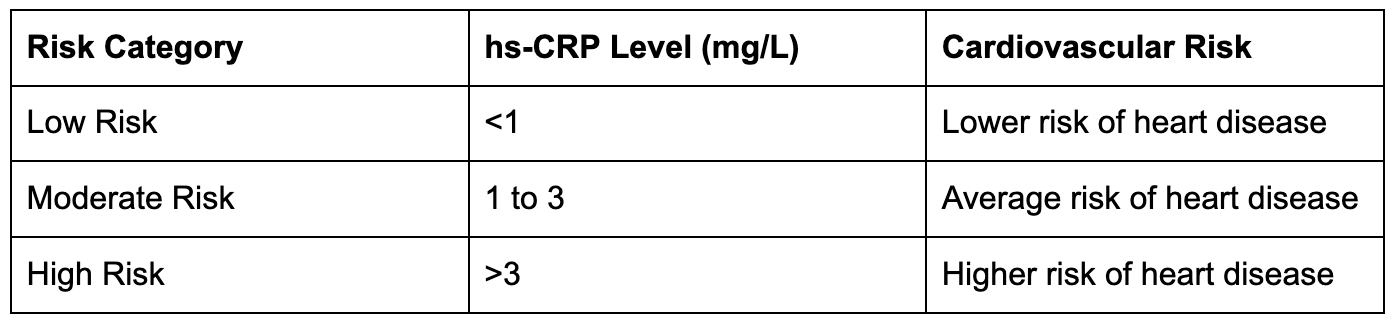
For example, a study in the Journal of the American Medical Association found that older adults with lower hs-CRP levels had a lower risk of dying over a 5-year period. Similarly, research involving elderly Chinese adults revealed that higher hs-CRP levels were linked to an increased risk of death from all causes. Below is a summary of cardiovascular risk categories based on hs-CRP levels:
Testing for hs-CRP is simple and widely accessible. A quick blood draw at clinics, labs, or hospitals can provide results in just a few days. How often you should test depends on your health goals and risk factors.
For example, if you're making changes to reduce inflammation, testing every 3–6 months can help you track progress and refine your approach.
In the U.S., the cost of hs-CRP testing varies but is often included in broader health assessments. Research shows that this test can identify up to 20% of individuals at high cardiovascular risk who might otherwise go undetected with standard screening methods. This makes it especially helpful for people who appear healthy but may have hidden risks.
If you're looking to lower your hs-CRP levels, these strategies can help:
The role of hs-CRP as a key biomarker for longevity is well-supported by research. A large study involving 27,939 women demonstrated that cardiovascular risks increased steadily with rising hs-CRP levels. Another study of 6,060 healthy Chinese participants found that hs-CRP levels rose with age, particularly after 45 years old. These findings highlight the importance of monitoring and managing hs-CRP as part of a broader strategy for healthy aging.
Keeping hs-CRP levels consistently low is associated with better physical and cognitive health as people age. Regular testing allows for early interventions, helping to prevent or manage inflammation-related diseases. For anyone focused on extending their healthspan, hs-CRP monitoring is a practical and impactful too.
A Complete Blood Count (CBC) is a simple yet crucial blood test that measures key components like haemoglobin, white blood cells (WBCs), and platelets. It’s not just useful for diagnosing immediate health concerns; it also helps track long-term patterns that are vital for maintaining overall health.
The CBC offers a snapshot of your overall health and can detect early warning signs of conditions that affect longevity, such as anaemia linked to chronic illnesses or certain blood cancers.
It’s also a tool for spotting chronic low-grade inflammation, which is tied to cardiovascular and metabolic diseases. For instance, a WBC count of 7,000 cells/mm³ or higher has been associated with a 2.3× increased risk of cardiovascular-related death.
Another valuable metric derived from a CBC is the neutrophil-to-lymphocyte ratio (NLR), which has been tied to higher overall mortality (HR: 1.14 per quartile) and heart disease mortality (HR: 1.17 per quartile).
Additionally, elevated red cell distribution width (RDW) levels are linked to a greater risk of vascular complications, heart failure, heart attack, stroke, and kidney issues.
One of the advantages of a CBC is its accessibility and affordability; it only requires a standard blood draw. For generally healthy individuals, an annual CBC is often sufficient. However, the frequency might need adjustment based on your health needs.
For example, individuals with autoimmune conditions or rheumatoid arthritis may require testing every three to six months, as guided by their healthcare provider.
CBC results provide clear, actionable insights. For example, even if your WBC count falls within the normal range, monitoring the NLR can help uncover chronic inflammation. Spotting elevated inflammatory markers early allow for timely interventions, like adopting anti-inflammatory diets or exercise routines. It’s important to discuss your specific results with your doctor, as optimal ranges can vary depending on individual health factors.
For those at risk of diabetes, RDW can be used alongside HbA1c and blood glucose levels to better predict the onset and complications of type 2 diabetes.
Research underscores the CBC's role in predicting cardiovascular risks. Elevated WBC counts, for example, have been found to pose risks similar to other inflammation markers like C-reactive protein.
Beyond identifying anaemia or blood cancers, the CBC offers vital insights into immune health and blood clotting, making it an indispensable tool for both aging and chronic disease prevention.
Your chronological age might tell you how many birthdays you've celebrated, but your biological age reveals the actual condition of your cells and tissues. This difference is crucial because biological age is a stronger predictor of age-related diseases, life expectancy, and overall health than the number of candles on your cake.
Unlike traditional health markers like blood sugar or cholesterol, biological age testing offers a more comprehensive picture of how your body is aging. And the best part? These tests provide actionable insights, helping you make lifestyle adjustments to potentially extend your healthy years.
Biological age testing has transformed how we assess health and aging risks. Unlike chronological age, your biological age can be reduced through lifestyle changes. This adaptability makes it a valuable tool for tracking your progress toward better health.
Research supports this, showing that a one-year increase in DNAm PhenoAge correlates with a 4.5% rise in all-cause mortality risk. Those in the fastest-aging group face a mortality hazard 1.62 times higher than average. At age 50, life expectancy varies significantly: 81 years for the fastest agers, 83.5 years for average agers, and 86 years for the slowest agers.
Advanced longevity panels are now easier to access, with many companies offering at-home kits or lab-based options at different price points. Blood-based biological age tests are particularly appealing since they are cost-effective and scalable compared to more complex methods like telomere testing. A simple blood draw similar to routine lab work can kick off the process, and periodic testing allows you to monitor changes as you tweak your lifestyle.
These tests act as a practical guide for making timely adjustments to live a healthier, longer life.
Biological age testing doesn’t just give you numbers; it provides a roadmap for improving your health. Research has shown that targeted interventions can reduce biological age by as much as six years. Key strategies include:
These interventions, combined with the insights from biological age testing, can help you craft a personalised health plan that aligns with your unique needs.
The research behind biological age testing is robust and growing. Advanced models that utilise 25 biomarkers can predict mortality with a C-Index of 0.778, outperforming traditional methods by up to 11%. Results can show a dramatic range, with biological ages differing by as much as 20 years younger or older than one's chronological age.
Among the available testing options, epigenetic tests demonstrate the strongest link to health outcomes, while single-marker tests like telomere length often show more variability. Tests that include a broad range of biomarkers tend to be more accurate, and AI-driven models are further improving precision by analysing complex data relationships.
The best part? Biological age is highly modifiable. Factors like diet, exercise, stress, sleep, and environment play a significant role in shaping your biological age. With the guidance of these tests, you hold the power to influence how you age and pave the way for a healthier future.
Curious how your body’s actual age compares to the calendar? Read our post on BioAge to discover what it means and how lifestyle choices can help close the gap.
The table below outlines essential longevity biomarkers, detailing their importance, ideal ranges, and practical strategies for improvement. Understanding these biomarkers can help you prioritise health tests and make informed lifestyle adjustments.
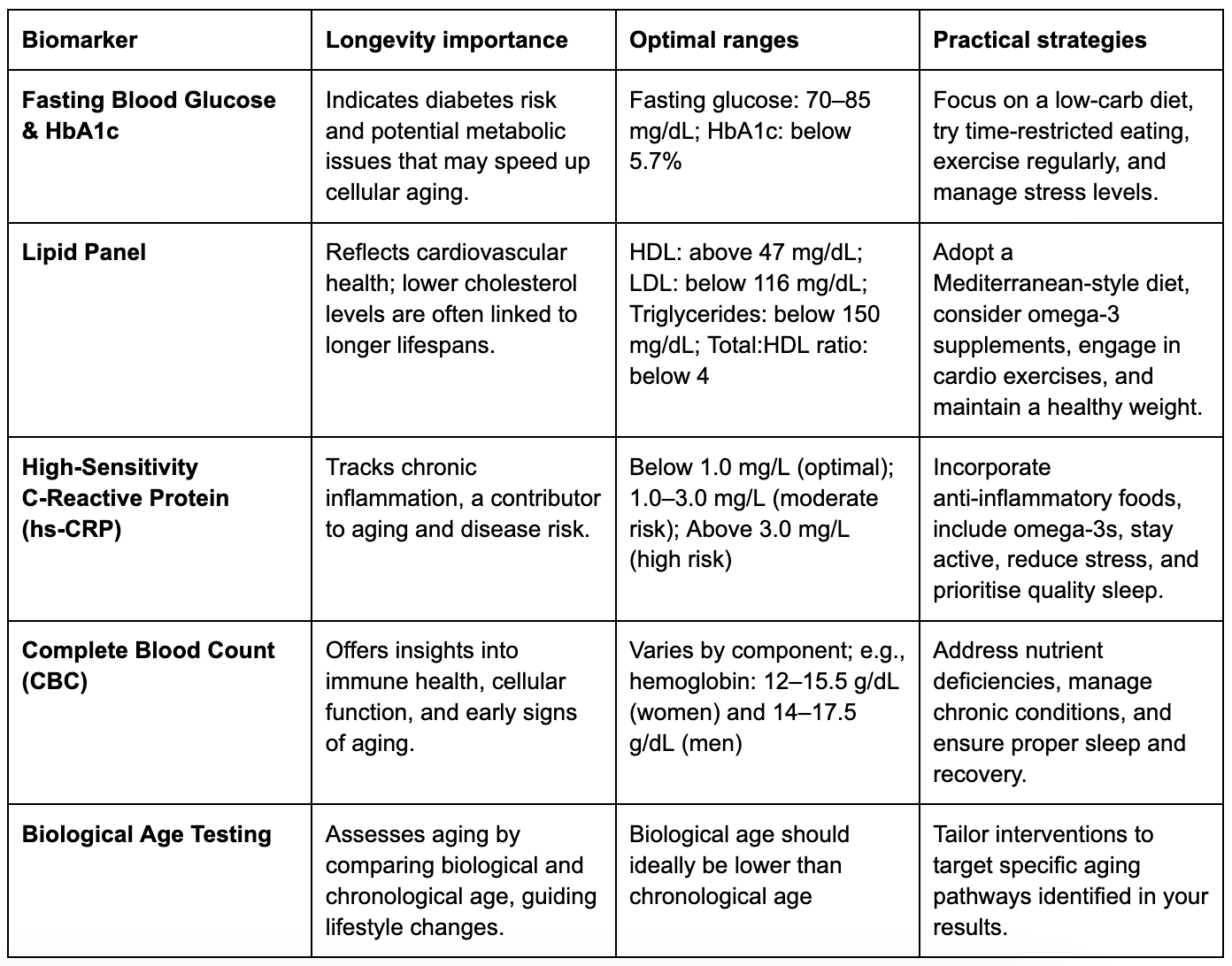
Regular testing of these biomarkers helps track your health over time, offering a clear picture of your metabolic and cardiovascular status. By monitoring trends, you can identify risks early and make adjustments to improve your healthspan.
Take, for instance, a person in their mid-40s with a history of cardiovascular disease. Through biomarker testing, they uncovered hidden risks and implemented targeted exercise and dietary changes. Over six months, they lost 20 pounds and reduced LDL cholesterol, ApoB, and fasting insulin levels by 20–30%.
To make the most of biomarker testing, choose tests that align with your health goals, family history, and budget. This proactive approach provides actionable insights and supports long-term well-being. Regular testing empowers you to take control of your health and extend your healthspan.
Tracking your longevity biomarkers is valuable, but making sense of the results and taking action is where the real impact happens. Vively uses continuous glucose monitoring (CGM) and personalised insights to help you optimise key markers like fasting glucose, HbA1c, and inflammation levels over time.
With Vively, you can:
By combining biomarker testing with Vively’s real-time data, you can take clear, measurable steps to improve your healthspan and stay healthier for longer.
Combining biomarker testing with modern monitoring tools offers an effective way to improve your healthspan and identify potential issues early. The five biomarkers we've discussed, fasting blood glucose and HbA1c, lipid panels, hs-CRP, complete blood count, and biological age testing paint a detailed picture of your metabolic health, inflammation levels, and the aging process.
On top of these tests, wearable devices now deliver real-time metabolic insights. Tools like continuous glucose monitors (CGMs) have changed the game, providing instant feedback on how your diet, exercise, and sleep habits influence your metabolic health. Pairing these tools with longevity panels that measure biological age gives you a deeper understanding of how your body is aging.
Wearables also encourage more physical activity, increasing daily steps by about 1,300 on average, and improve the effectiveness of health coaching. The wearable healthcare market is expected to grow to $69.2 billion by 2028. Together, regular biomarker testing, continuous monitoring through devices like CGMs, and personalised coaching offer a proactive approach to optimising your health, shifting the focus from treating illnesses to preventing them.
Talk with your healthcare provider about these biomarkers, and consider incorporating advanced monitoring tools into your health plan.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Want to stay healthier for longer? Testing key biomarkers can help you understand how your body is aging and identify areas to improve your healthspan. Here are five tests that provide actionable insights:
Fasting blood glucose (FBG) and HbA1c are two essential markers for understanding blood sugar control. They provide insights into both short-term and long-term glucose levels, which are crucial for maintaining overall health and longevity.
Keeping blood sugar levels in check plays a big role in healthy aging. Elevated blood sugar can significantly shorten healthspan. For instance, research shows that a one standard deviation increase in HbA1c is linked to a 29% higher chance of healthspan ending prematurely. On top of that, every 1% increase in HbA1c above 6% raises the risk of cardiovascular disease by 18%.
FBG provides a quick snapshot of blood sugar levels after fasting for 8–12 hours, while HbA1c reflects the average blood sugar levels over the past 2–3 months. Elevated HbA1c is not only a marker for diabetes but is also an independent risk factor for coronary heart disease and stroke.
Additionally, genetic tendencies toward higher fasting blood glucose are associated with a 5% increased risk of developing chronic diseases.
Both FBG and HbA1c tests are straightforward and widely available. FBG requires fasting for 8 to 12 hours before a blood draw, while HbA1c testing can be done at any time without fasting.
How often should you test?
Advanced tools like continuous glucose monitors (CGMs) provide real-time data, though they come with higher costs. Considering that over a third of U.S. adults have prediabetes, most without knowing it. CGMs can help uncover hidden blood sugar trends.
Healthy glucose levels are key to long-term wellbeing. An HbA1c level between 5.7% and 6.4% signals prediabetes, while a level of 6.5% or higher on two separate tests confirms diabetes. HbA1c is a more reliable indicator of long-term glucose control compared to fasting blood glucose, as it isn’t easily influenced by short-term factors like illness or stress.
Lifestyle changes can make a big difference in glucose management. Diet, exercise, and medical care all play a role in maintaining a healthy metabolic profile.
Some effective dietary tips include:
Physical activity and regular meal patterns also help regulate blood sugar levels.
For those using CGMs, these devices can integrate with sleep and stress data to predict glucose changes and provide alerts for timely intervention. When combined with stress management techniques and consistent monitoring, these strategies can significantly improve metabolic health and support a longer, healthier life.
Want to take your health tracking a step further? Check out our guide on improving blood markers naturally from CRP to HbA1c to see how small lifestyle changes add up.
A lipid panel measures four key markers: total cholesterol, LDL (low-density lipoprotein), HDL (high-density lipoprotein), and triglycerides. These numbers provide valuable insight into cardiovascular health and overall longevity.
An unhealthy lipid profile characterised by high LDL and triglycerides alongside low HDL is a significant risk factor for cardiovascular disease. Since heart disease is the leading cause of death in the United States, keeping these markers in check plays a critical role in maintaining a longer, healthier life.
High LDL levels are closely linked to atherosclerosis, which can lead to cardiovascular complications. Additionally, smaller LDL particle sizes are associated with higher risks of type 2 diabetes, metabolic syndrome, and coronary artery disease.
HDL, often called "good cholesterol", helps protect against heart disease by reducing inflammation and preventing LDL oxidation. On the other hand, elevated triglycerides are a hallmark of metabolic syndrome, which increases the likelihood of cardiovascular disease and type 2 diabetes. The triglyceride-to-HDL ratio is particularly telling; it’s a strong indicator of type 2 diabetes risk
Another useful metric is the total cholesterol to HDL ratio, which many studies suggest is a better predictor of heart disease than LDL alone. Ideally, this ratio should be 5:1 or lower, with 3.5:1 being the optimal target.
Regular lipid testing is straightforward, accessible, and affordable. It can be done at a doctor’s office, lab, clinic, or hospital, usually through a standard blood draw. Results are typically available quickly, making it easy to track changes over time.
Testing frequency depends on individual risk factors. Those with a family history of heart disease, diabetes, high blood pressure, or other risks such as smoking or obesity should monitor their levels more often. A healthcare provider can recommend an appropriate schedule based on your age and risk profile.
Cost isn’t a barrier for most people. Lipid panel tests at walk-in clinics or pharmacies often cost under $100. For added convenience, point-of-care testing using a finger prick or at-home kits offers quicker results, though these methods may not always provide the same level of accuracy as traditional lab tests.
Improving your lipid profile doesn’t require drastic measures. Consistent lifestyle changes can make a big difference.
By combining these strategies, you can support heart health and promote overall metabolic balance, key factors in extending your healthspan.
Research underscores the importance of lipid management in preventing chronic disease and promoting longevity. For instance, elevated Lp(a), a cholesterol particle linked to cardiovascular risk, affects approximately 1.5 billion people globally. With over 90% of Lp(a) levels determined by genetics, it’s the most common form of inherited dyslipidaemia.
Testing for Lp(a) is relatively affordable, ranging from $25 to $100, similar to standard lipid panels.
Regularly monitoring and optimising your lipid levels is a powerful way to reduce the risk of age-related chronic diseases and improve your long-term health outlook. By staying proactive, you can take meaningful steps toward a healthier, longer life.
Want to understand how hidden inflammation might be slowing you down? Read our article on chronic inflammation and the CRP blood test that reveals it.
High-sensitivity C-reactive protein (hs-CRP) is a test that measures even the smallest levels of inflammation in the body, offering more detailed insights compared to standard CRP tests. It serves as a reliable marker for chronic inflammation, which has been closely linked to aging and various chronic conditions.
Chronic inflammation, often termed "inflammaging", plays a key role in the aging process and contributes to the onset of age-related diseases. CRP is produced by the liver in response to inflammation, infections, or tissue damage. Research shows that hs-CRP levels above 3 mg/L can reduce life expectancy by up to 4 years, while keeping levels below 1 mg/L may extend lifespan by 8–10 years. Elevated hs-CRP levels are also strongly associated with a higher risk of cardiovascular disease and shorter lifespans.
For example, a study in the Journal of the American Medical Association found that older adults with lower hs-CRP levels had a lower risk of dying over a 5-year period. Similarly, research involving elderly Chinese adults revealed that higher hs-CRP levels were linked to an increased risk of death from all causes. Below is a summary of cardiovascular risk categories based on hs-CRP levels:
Testing for hs-CRP is simple and widely accessible. A quick blood draw at clinics, labs, or hospitals can provide results in just a few days. How often you should test depends on your health goals and risk factors.
For example, if you're making changes to reduce inflammation, testing every 3–6 months can help you track progress and refine your approach.
In the U.S., the cost of hs-CRP testing varies but is often included in broader health assessments. Research shows that this test can identify up to 20% of individuals at high cardiovascular risk who might otherwise go undetected with standard screening methods. This makes it especially helpful for people who appear healthy but may have hidden risks.
If you're looking to lower your hs-CRP levels, these strategies can help:
The role of hs-CRP as a key biomarker for longevity is well-supported by research. A large study involving 27,939 women demonstrated that cardiovascular risks increased steadily with rising hs-CRP levels. Another study of 6,060 healthy Chinese participants found that hs-CRP levels rose with age, particularly after 45 years old. These findings highlight the importance of monitoring and managing hs-CRP as part of a broader strategy for healthy aging.
Keeping hs-CRP levels consistently low is associated with better physical and cognitive health as people age. Regular testing allows for early interventions, helping to prevent or manage inflammation-related diseases. For anyone focused on extending their healthspan, hs-CRP monitoring is a practical and impactful too.
A Complete Blood Count (CBC) is a simple yet crucial blood test that measures key components like haemoglobin, white blood cells (WBCs), and platelets. It’s not just useful for diagnosing immediate health concerns; it also helps track long-term patterns that are vital for maintaining overall health.
The CBC offers a snapshot of your overall health and can detect early warning signs of conditions that affect longevity, such as anaemia linked to chronic illnesses or certain blood cancers.
It’s also a tool for spotting chronic low-grade inflammation, which is tied to cardiovascular and metabolic diseases. For instance, a WBC count of 7,000 cells/mm³ or higher has been associated with a 2.3× increased risk of cardiovascular-related death.
Another valuable metric derived from a CBC is the neutrophil-to-lymphocyte ratio (NLR), which has been tied to higher overall mortality (HR: 1.14 per quartile) and heart disease mortality (HR: 1.17 per quartile).
Additionally, elevated red cell distribution width (RDW) levels are linked to a greater risk of vascular complications, heart failure, heart attack, stroke, and kidney issues.
One of the advantages of a CBC is its accessibility and affordability; it only requires a standard blood draw. For generally healthy individuals, an annual CBC is often sufficient. However, the frequency might need adjustment based on your health needs.
For example, individuals with autoimmune conditions or rheumatoid arthritis may require testing every three to six months, as guided by their healthcare provider.
CBC results provide clear, actionable insights. For example, even if your WBC count falls within the normal range, monitoring the NLR can help uncover chronic inflammation. Spotting elevated inflammatory markers early allow for timely interventions, like adopting anti-inflammatory diets or exercise routines. It’s important to discuss your specific results with your doctor, as optimal ranges can vary depending on individual health factors.
For those at risk of diabetes, RDW can be used alongside HbA1c and blood glucose levels to better predict the onset and complications of type 2 diabetes.
Research underscores the CBC's role in predicting cardiovascular risks. Elevated WBC counts, for example, have been found to pose risks similar to other inflammation markers like C-reactive protein.
Beyond identifying anaemia or blood cancers, the CBC offers vital insights into immune health and blood clotting, making it an indispensable tool for both aging and chronic disease prevention.
Your chronological age might tell you how many birthdays you've celebrated, but your biological age reveals the actual condition of your cells and tissues. This difference is crucial because biological age is a stronger predictor of age-related diseases, life expectancy, and overall health than the number of candles on your cake.
Unlike traditional health markers like blood sugar or cholesterol, biological age testing offers a more comprehensive picture of how your body is aging. And the best part? These tests provide actionable insights, helping you make lifestyle adjustments to potentially extend your healthy years.
Biological age testing has transformed how we assess health and aging risks. Unlike chronological age, your biological age can be reduced through lifestyle changes. This adaptability makes it a valuable tool for tracking your progress toward better health.
Research supports this, showing that a one-year increase in DNAm PhenoAge correlates with a 4.5% rise in all-cause mortality risk. Those in the fastest-aging group face a mortality hazard 1.62 times higher than average. At age 50, life expectancy varies significantly: 81 years for the fastest agers, 83.5 years for average agers, and 86 years for the slowest agers.
Advanced longevity panels are now easier to access, with many companies offering at-home kits or lab-based options at different price points. Blood-based biological age tests are particularly appealing since they are cost-effective and scalable compared to more complex methods like telomere testing. A simple blood draw similar to routine lab work can kick off the process, and periodic testing allows you to monitor changes as you tweak your lifestyle.
These tests act as a practical guide for making timely adjustments to live a healthier, longer life.
Biological age testing doesn’t just give you numbers; it provides a roadmap for improving your health. Research has shown that targeted interventions can reduce biological age by as much as six years. Key strategies include:
These interventions, combined with the insights from biological age testing, can help you craft a personalised health plan that aligns with your unique needs.
The research behind biological age testing is robust and growing. Advanced models that utilise 25 biomarkers can predict mortality with a C-Index of 0.778, outperforming traditional methods by up to 11%. Results can show a dramatic range, with biological ages differing by as much as 20 years younger or older than one's chronological age.
Among the available testing options, epigenetic tests demonstrate the strongest link to health outcomes, while single-marker tests like telomere length often show more variability. Tests that include a broad range of biomarkers tend to be more accurate, and AI-driven models are further improving precision by analysing complex data relationships.
The best part? Biological age is highly modifiable. Factors like diet, exercise, stress, sleep, and environment play a significant role in shaping your biological age. With the guidance of these tests, you hold the power to influence how you age and pave the way for a healthier future.
Curious how your body’s actual age compares to the calendar? Read our post on BioAge to discover what it means and how lifestyle choices can help close the gap.
The table below outlines essential longevity biomarkers, detailing their importance, ideal ranges, and practical strategies for improvement. Understanding these biomarkers can help you prioritise health tests and make informed lifestyle adjustments.
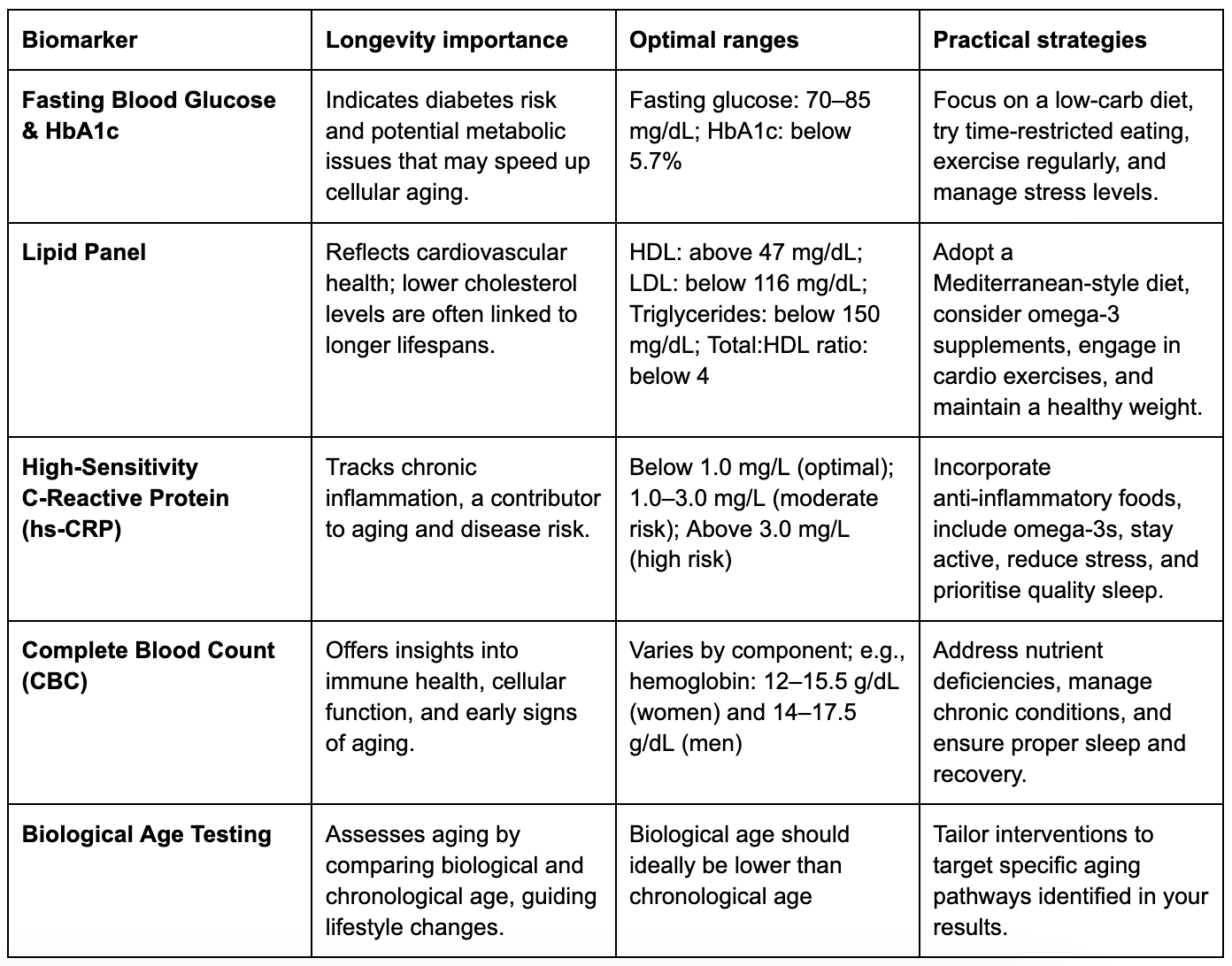
Regular testing of these biomarkers helps track your health over time, offering a clear picture of your metabolic and cardiovascular status. By monitoring trends, you can identify risks early and make adjustments to improve your healthspan.
Take, for instance, a person in their mid-40s with a history of cardiovascular disease. Through biomarker testing, they uncovered hidden risks and implemented targeted exercise and dietary changes. Over six months, they lost 20 pounds and reduced LDL cholesterol, ApoB, and fasting insulin levels by 20–30%.
To make the most of biomarker testing, choose tests that align with your health goals, family history, and budget. This proactive approach provides actionable insights and supports long-term well-being. Regular testing empowers you to take control of your health and extend your healthspan.
Tracking your longevity biomarkers is valuable, but making sense of the results and taking action is where the real impact happens. Vively uses continuous glucose monitoring (CGM) and personalised insights to help you optimise key markers like fasting glucose, HbA1c, and inflammation levels over time.
With Vively, you can:
By combining biomarker testing with Vively’s real-time data, you can take clear, measurable steps to improve your healthspan and stay healthier for longer.
Combining biomarker testing with modern monitoring tools offers an effective way to improve your healthspan and identify potential issues early. The five biomarkers we've discussed, fasting blood glucose and HbA1c, lipid panels, hs-CRP, complete blood count, and biological age testing paint a detailed picture of your metabolic health, inflammation levels, and the aging process.
On top of these tests, wearable devices now deliver real-time metabolic insights. Tools like continuous glucose monitors (CGMs) have changed the game, providing instant feedback on how your diet, exercise, and sleep habits influence your metabolic health. Pairing these tools with longevity panels that measure biological age gives you a deeper understanding of how your body is aging.
Wearables also encourage more physical activity, increasing daily steps by about 1,300 on average, and improve the effectiveness of health coaching. The wearable healthcare market is expected to grow to $69.2 billion by 2028. Together, regular biomarker testing, continuous monitoring through devices like CGMs, and personalised coaching offer a proactive approach to optimising your health, shifting the focus from treating illnesses to preventing them.
Talk with your healthcare provider about these biomarkers, and consider incorporating advanced monitoring tools into your health plan.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
