Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan




Vitamin D deficiency is a global issue, affecting 1 billion people worldwide, including 35% of U.S. adults.
It’s linked to brittle bones, muscle weakness, and a weakened immune system. Key causes include limited sunlight, poor diet, and absorption problems. High-risk groups include older adults, people with darker skin, and those with certain medical conditions.
Understanding your vitamin D levels and addressing deficiencies early can help prevent serious health complications. Consult a healthcare provider for personalised advice.
Vitamin D pulls double duty as both a vitamin and a hormone, playing a crucial role in maintaining overall health. One of its main jobs is helping your body absorb calcium and phosphorus, which are essential for building and maintaining strong bones.
Beyond bone health, vitamin D supports your immune system, nervous system, and musculoskeletal health. It helps your intestines absorb calcium, mobilises calcium from bones when needed, and aids in kidney calcium reabsorption.
On top of that, vitamin D is involved in regulating insulin sensitivity and energy balance, which are key for metabolic health. A deficiency in vitamin D can lead to serious conditions like rickets in children, osteomalacia in adults, and weakened immune responses.
Recognising the many ways vitamin D supports your body underscores why it's so important to get enough of it. Let’s explore how you can do just that.
Australians primarily obtain vitamin D through sunlight, food, and supplements. Sunlight is the most natural source, as UVB rays trigger the production of vitamin D3 in your skin. However, this process isn’t always straightforward. Factors like sunscreen use, limited outdoor time, and darker skin tones can reduce your body’s ability to produce vitamin D.
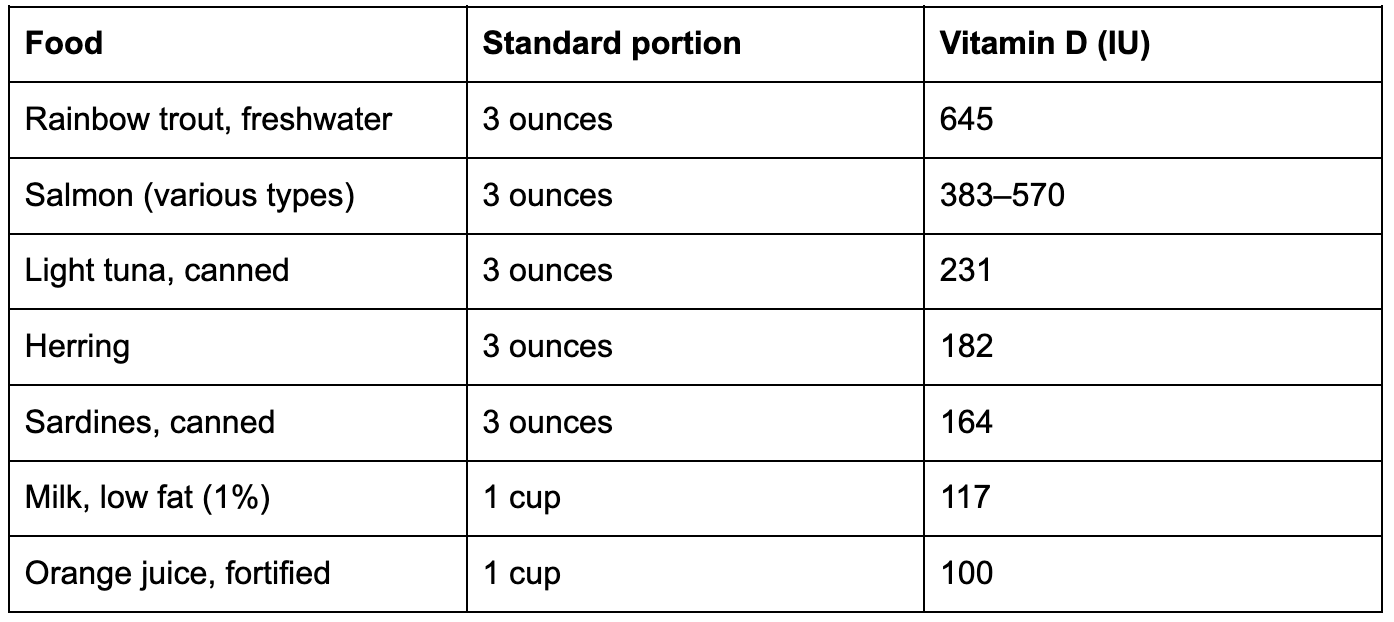
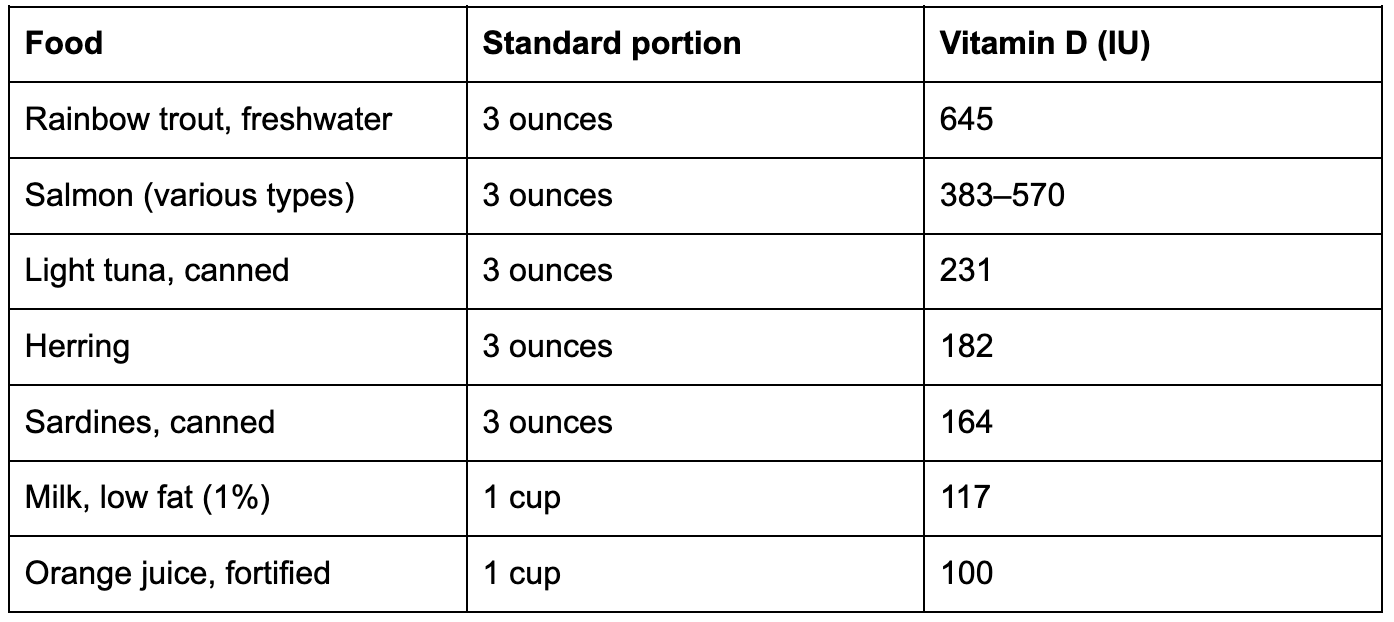
Diet and supplements help fill the gap. While only a few foods naturally contain vitamin D, some are fortified to help meet daily needs. Here’s a quick look at some key dietary sources:
Supplements are another reliable way to maintain healthy vitamin D levels. They come in two forms: D2 (ergocalciferol), derived from plants, and D3 (cholecalciferol), which is naturally produced in your body and found in animal-based foods.
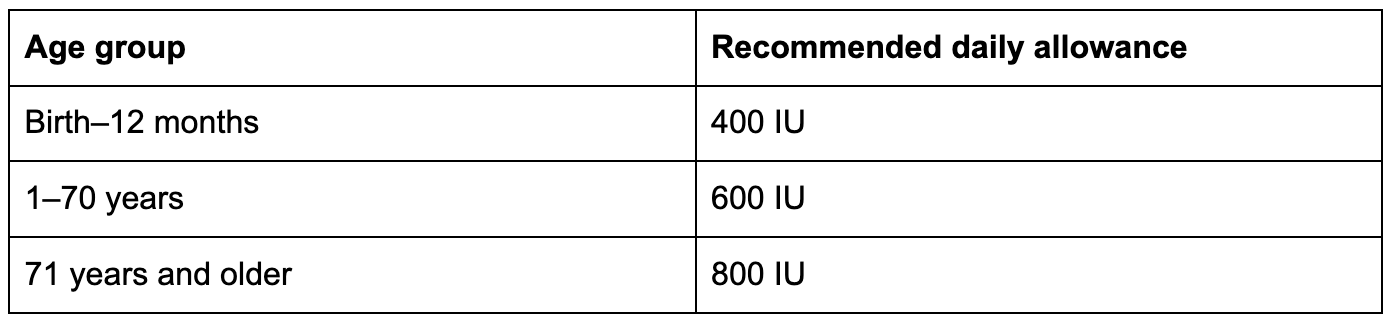
D3 is generally better at raising and maintaining blood vitamin D levels. For adults aged 19–70, the recommended daily intake is 600 IU (15 mcg), increasing to 800 IU (20 mcg) for those over 70. The upper safe limit is 4,000 IU (100 mcg) per day.
If you have minimal sun exposure or darker skin, a daily supplement of 1,000 to 2,000 IU might be a smart choice.
Vitamin D deficiency often sneaks in under the radar, disguising itself as everyday fatigue or stress. Many people chalk up their tiredness to the demands of daily life, unaware that their vitamin D levels might be dropping. These subtle and vague symptoms make it easy for a deficiency to go unnoticed.
Knowing what to watch for can help you catch this issue early, before it has a more serious impact on your health. Below, we’ll explore the key physical and mental warning signs, as well as the groups most at risk.
The symptoms of vitamin D deficiency can vary, but they often include fatigue, bone pain, and muscle issues. Fatigue is usually the first sign, but it’s easy to dismiss as a result of overworking or stress. Other physical symptoms include bone pain, muscle weakness, cramps, or general aches. These occur because vitamin D is essential for calcium absorption and muscle function.
Mental health can also take a hit. A deficiency in vitamin D has been linked to mood changes, including depression or persistent sadness. This makes sense, as vitamin D receptors are found throughout the brain and nervous system.
Interestingly, many people with vitamin D deficiency show no symptoms at all. If you’re dealing with unexplained fatigue and can’t pinpoint the cause—like illness or poor sleep—it might be worth getting your vitamin D levels tested.
Some groups are more likely to experience vitamin D deficiency due to factors like skin tone, age, lifestyle, or where they live. For example, people with darker skin are at a higher risk because melanin reduces the skin’s ability to produce vitamin D from sunlight.
Research shows that African-Americans need up to six times more UVB exposure than those with lighter skin to produce the same amount of vitamin D.
Age is another significant factor. Among seniors, deficiency rates range from 15% to 52%, with those in nursing homes being particularly vulnerable. In Sydney, for instance, 86% of women and 68% of men in nursing homes were found to have moderate deficiencies. Younger people aren’t immune either—17% of teenagers and 32% of young adults are deficient.
Geography and lifestyle also play a role. Urban areas report higher deficiency rates (27%) compared to inner regional (16%), outer regional (13%), and remote areas (9%). This urban-rural gap likely reflects differences in sun exposure and outdoor activities.
Certain ethnicities face higher risks too. For example, deficiency rates are high among individuals born in Southern and Central Asia (67%), Northeast Asia (64%), Southeast Asia (58%), and North Africa and the Middle East (50%).
Other high-risk groups include people who cover their skin for religious or cultural reasons, those with limited outdoor time due to work or lifestyle, and individuals with health conditions like obesity, PCOS, or insulin resistance. Interestingly, Australia’s "sun smart" campaign, while reducing sunburn rates, has also coincided with a rise in vitamin D deficiencies.
Regular checkups with a healthcare provider can help ensure your vitamin D levels are where they need to be—ideally before symptoms even start.
Looking to support your energy, mood, or cycle? Check out our guide to the best supplements for balancing hormones in Australia.
When your vitamin D levels dip, your body starts signalling trouble, often in ways that can range from subtle to serious. These issues can affect everything from your bones to your immune system.
Recognising the signs early can help you address potential problems before they escalate. Let’s take a closer look at how low vitamin D impacts different parts of the body.
Low vitamin D can affect your body right away or over time. Early signs include fatigue and low immunity, while long-term deficiency may lead to bone issues and chronic disease risk.
Your bones are the first to feel the effects of a vitamin D deficiency. Without enough vitamin D, your body struggles to absorb calcium effectively, setting off a chain reaction of bone-related issues. Even a mild, ongoing deficiency can lead to hypocalcaemia and secondary hyperparathyroidism, both of which increase the likelihood of osteoporosis, falls, and fractures.
In children, severe vitamin D deficiency can result in rickets, a condition characterised by abnormal growth, muscle weakness, bone pain, and joint deformities. For adults, the problem can progress to osteomalacia, where bones become soft and brittle, significantly raising the risk of fractures.
A lack of vitamin D can leave your immune system vulnerable, making you more prone to infections and autoimmune disorders.
Low vitamin D levels have been linked to a higher risk of cardiovascular disease and type 2 diabetes. Additionally, obesity increases the prevalence of vitamin D deficiency by 35%, creating a harmful cycle that’s tough to break.
Low levels of 25-hydroxyvitamin D are associated with a 30%–50% higher risk of developing colon, prostate, and breast cancers, along with increased cancer-related mortality.
Vitamin D deficiency has been connected to depression and mood disorders. Since vitamin D receptors are present throughout the brain and nervous system, insufficient levels may negatively affect mood, mental clarity, and overall cognitive health.
Understanding the severity of a deficiency can help guide appropriate treatment:
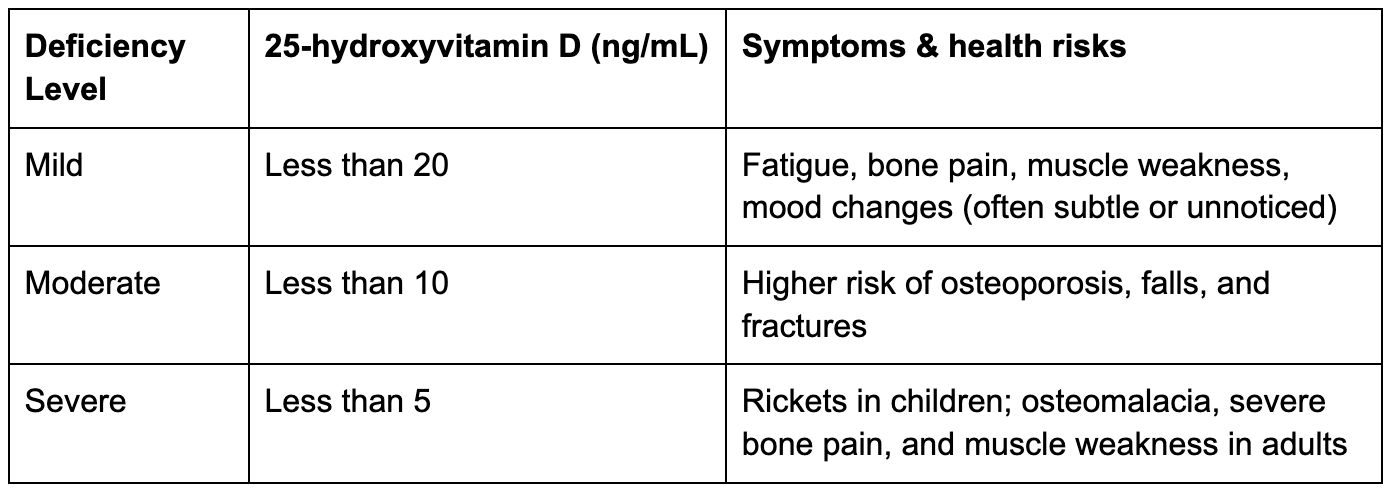
Mild deficiency can be easy to overlook. You might feel more tired than usual or have muscle aches that are mistaken for stress or overexertion. For children, even a mild deficiency might cause weak or sore muscles.
Severe deficiency, on the other hand, is much harder to ignore. Children may develop rickets, leading to visible bone deformities, while adults face osteomalacia with symptoms like soft, weak bones and significant pain. Older adults with vitamin D levels below 10 ng/mL are at a much greater risk of experiencing dangerous falls.
Addressing a deficiency early, whether mild or severe, can prevent these complications from becoming life-altering. Proper detection and treatment make all the difference.
Testing for vitamin D deficiency starts with recognising risk factors and symptoms. Knowing when to take this step can help catch potential problems early.
Doctors often recommend testing when patients report symptoms linked to vitamin D deficiency. These may include bone or muscle pain, increased sensitivity to pain, tingling sensations, muscle weakness, or a history of fractures.
Some medical conditions can interfere with how your body absorbs or processes vitamin D. These include cystic fibrosis, Crohn's disease, coeliac disease, obesity, kidney disease, and liver disease. If you have any of these, regular monitoring might be necessary.
Certain medications, like steroids, cholesterol-lowering drugs, seizure medications, rifampin, and orlistat, can reduce vitamin D levels over time. If you're on these medications, talk to your doctor about monitoring your levels.
Infants, especially those who are breastfed, and older adults, whose skin produces less vitamin D, are advised to undergo regular testing.
If you fall into any of these categories or are experiencing symptoms, the next step is to understand how to interpret your test results.
Curious about your cardiovascular fitness? Explore our complete guide to VO₂ max and how it connects to your long-term health goals.
Testing for vitamin D is straightforward. It typically involves a blood draw (or a finger prick/heel stick for infants), with results available within a few business days. No special preparation is required, though you should inform your doctor of any medications or supplements you’re taking.
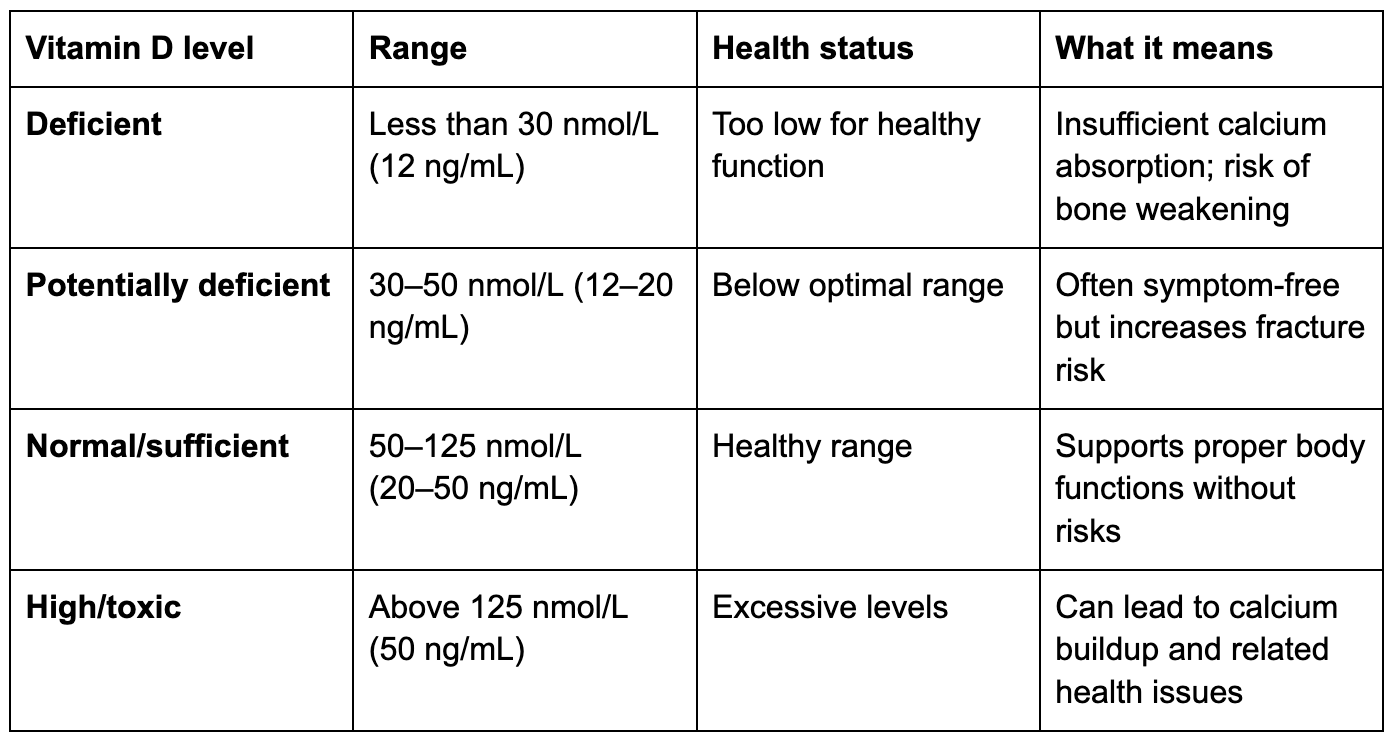
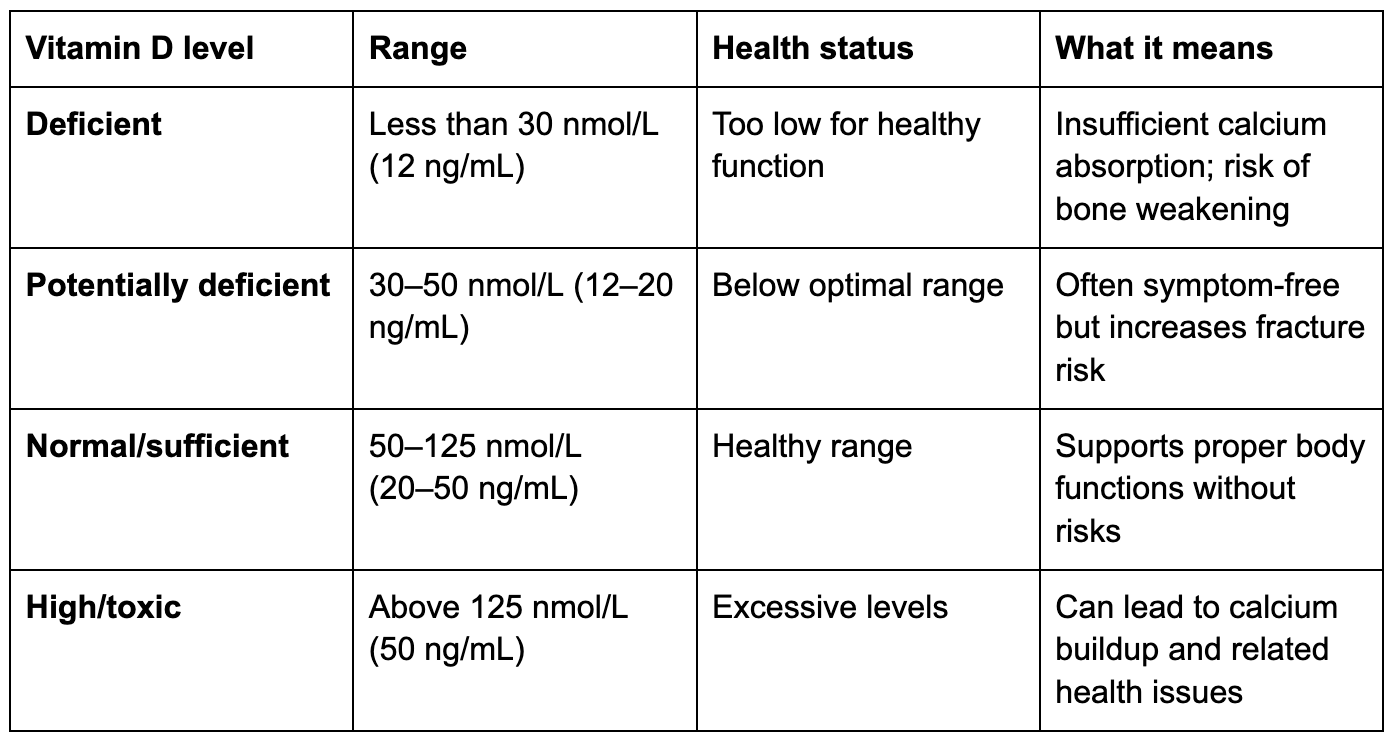
Vitamin D levels are measured as 25-hydroxy concentrations in either nanomoles per liter (nmol/L) or nanograms per milliliter (ng/mL). Here's how the results are categorised:
What to ask your doctor
Once you have your results, discuss them with your healthcare provider. Key questions might include:
If your levels are low, your doctor may recommend dietary changes or supplements. On the other hand, if your levels are high, stop taking supplements immediately and consult your doctor.
Testing costs vary depending on the provider. Out-of-pocket expenses can range from $75 to $99, though many insurance plans cover the test if it’s medically necessary.
Want to learn how your habits are shaping your long-term health? Check out our guide on what your BioAge really means and how to improve it.
Once you’ve identified your vitamin D levels, it’s time to take steps to improve them. A combination of safe sun exposure, dietary adjustments, and supplements can help you get back on track.
Sunlight is the most natural way to boost vitamin D, but how much you need depends on factors like location, skin tone, and the time of year.
Where you live significantly impacts how much sunlight you need. For example, someone in Miami during the summer might only need 3 minutes of sun exposure with 25% of their skin exposed, while the same person would require 23 minutes at noon in Boston during winter. This explains why vitamin D deficiency is more common in northern states during the colder months.
Skin tone plays a big role in how much sun exposure is necessary. While 4–15 minutes of midday sun may work for lighter skin tones, individuals with darker skin need more time due to higher melanin levels, which naturally block UV rays and slow vitamin D production.
To safely benefit from the sun, expose your skin during midday when UVB rays are strongest. After 10–30 minutes of unprotected exposure, apply sunscreen to prevent burns. Keep in mind that UVB rays don’t penetrate glass, so sitting by a sunny window won’t help.
Interestingly, sunscreen doesn’t completely block UVB rays. Research shows that 15.6% of UV radiation still reaches the skin, even with sunscreen.
Beyond sunlight, you can turn to food and supplements to ensure your vitamin D levels stay optimal.
Since only a few foods naturally contain vitamin D, fatty fish is a great option. For instance, a 3.5-ounce serving of farmed Atlantic salmon provides 441 IU of vitamin D, while wild-caught salmon often offers even more.
Many everyday foods in Australia are fortified with vitamin D to make it easier to meet your needs. For example:
For plant-based eaters, UV-treated mushrooms are a fantastic source of vitamin D. A single cup of cremini mushrooms exposed to UV light packs 1,100 IU of vitamin D - 139% of the daily value. These mushrooms are becoming more widely available in grocery stores.
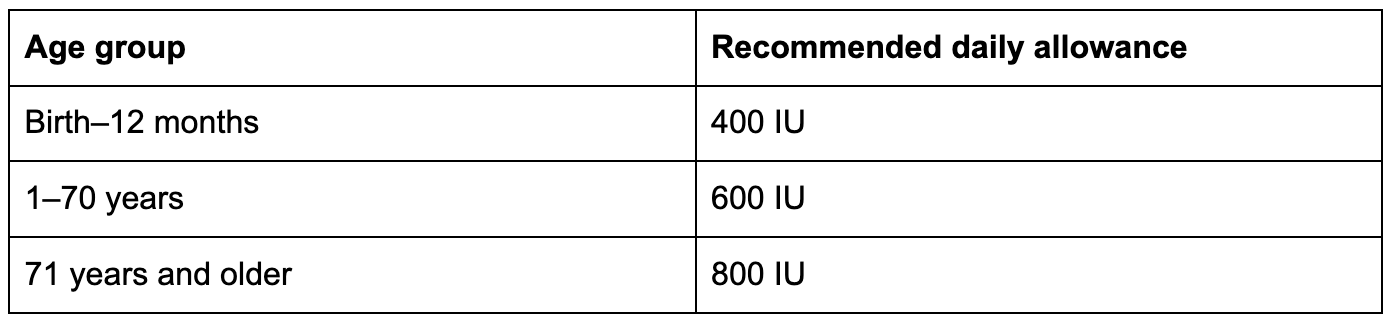
If food and sunlight aren’t enough, supplements can fill the gap. Vitamin D3 (cholecalciferol) is more effective than D2 at raising blood vitamin D levels. The recommended daily allowance varies by age:
Look for third-party tested supplements to ensure quality.
For a more comprehensive approach, consider combining these strategies with tools that monitor your overall health.
Addressing vitamin D deficiency isn’t just about bone health—it also supports your metabolism. Vitamin D plays a role in how your body processes nutrients and maintains energy balance. This makes it a great time to adopt a holistic approach by tracking other aspects of your health.
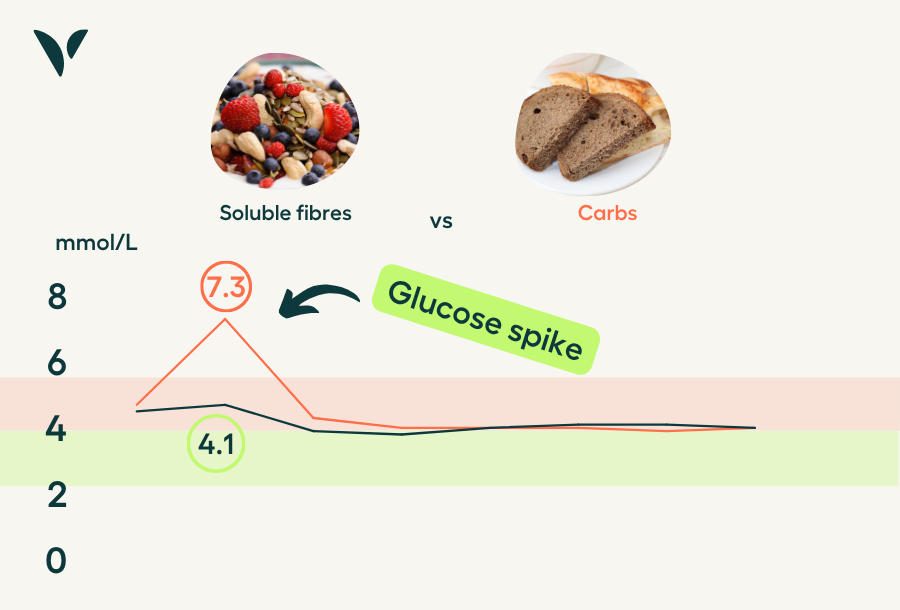
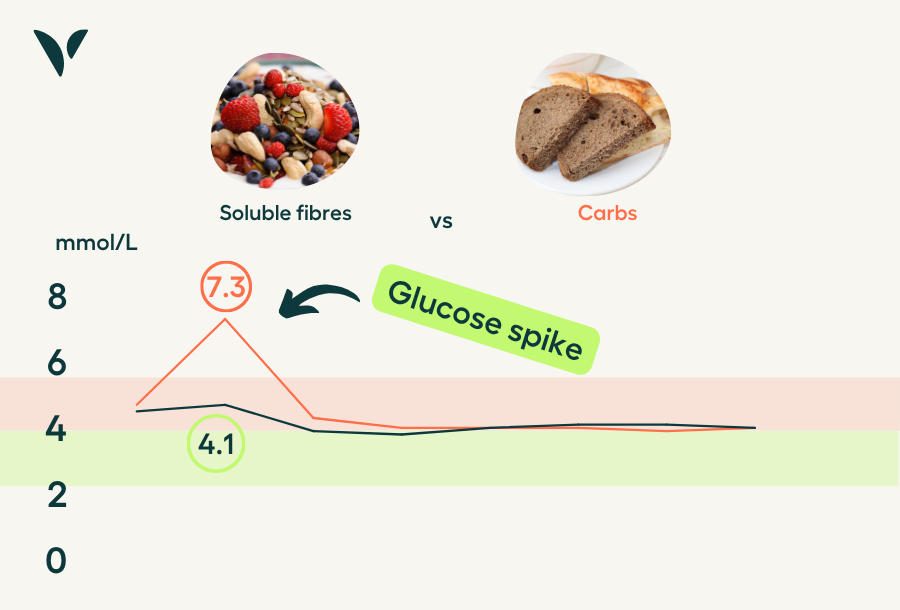
Health tracking tools can show how improving vitamin D levels impacts your overall metabolic health. Platforms like Vively, which offer continuous glucose monitoring (CGM), let you see real-time data on how dietary changes like adding vitamin D-rich foods or supplements affect your glucose levels and metabolic function.
The lifestyle changes that help with vitamin D deficiency, like midday sun exposure, eating nutrient-packed foods, and sticking to a supplement routine, often benefit your metabolism as well. By using health monitoring tools, you can track how these changes positively influence your overall health.
When you’re already working on improving your vitamin D levels, it’s the perfect time to implement other health strategies. With continuous monitoring, you can identify which dietary choices work best for your body, optimising both your vitamin D levels and your metabolic health.
Managing your vitamin D levels through sunlight, food, and supplements is a great step, but it also helps to see how these changes fit into your bigger health picture. Vively gives you real-time insights into your metabolic health so you can make informed decisions every day.
With Vively, you can:
Vitamin D affects more than bone health—it also plays a role in metabolism and energy regulation. Vively helps you stay in tune with your body and create habits that truly support your wellbeing.
Vitamin D deficiency affects a large portion of the population. By combining safe sun exposure, a nutrient-packed diet, and supplements, you can take control of your vitamin D levels and support overall health.
Try to get 15–30 minutes of sun exposure a few times a week, include foods like fatty fish and fortified products in your meals, and consider adding vitamin D₃ supplements to your routine.
Your specific needs depend on factors like your skin tone, age, location, and daily habits. The Endocrine Society suggests most healthy adults aim for 1,500 to 2,000 IU per day, but consulting a healthcare provider is the best way to tailor this to your situation.
The encouraging part? Vitamin D deficiency is manageable with the right approach. For better absorption, take your vitamin D supplements with meals that include healthy fats. Additionally, tools like continuous glucose monitors can offer insights into how optimising vitamin D levels benefits your overall metabolic health.
Taking steps to balance your vitamin D levels now can lead to stronger bones, a healthier immune system, and better metabolic well-being.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Vitamin D deficiency is a global issue, affecting 1 billion people worldwide, including 35% of U.S. adults.
It’s linked to brittle bones, muscle weakness, and a weakened immune system. Key causes include limited sunlight, poor diet, and absorption problems. High-risk groups include older adults, people with darker skin, and those with certain medical conditions.
Understanding your vitamin D levels and addressing deficiencies early can help prevent serious health complications. Consult a healthcare provider for personalised advice.
Vitamin D pulls double duty as both a vitamin and a hormone, playing a crucial role in maintaining overall health. One of its main jobs is helping your body absorb calcium and phosphorus, which are essential for building and maintaining strong bones.
Beyond bone health, vitamin D supports your immune system, nervous system, and musculoskeletal health. It helps your intestines absorb calcium, mobilises calcium from bones when needed, and aids in kidney calcium reabsorption.
On top of that, vitamin D is involved in regulating insulin sensitivity and energy balance, which are key for metabolic health. A deficiency in vitamin D can lead to serious conditions like rickets in children, osteomalacia in adults, and weakened immune responses.
Recognising the many ways vitamin D supports your body underscores why it's so important to get enough of it. Let’s explore how you can do just that.
Australians primarily obtain vitamin D through sunlight, food, and supplements. Sunlight is the most natural source, as UVB rays trigger the production of vitamin D3 in your skin. However, this process isn’t always straightforward. Factors like sunscreen use, limited outdoor time, and darker skin tones can reduce your body’s ability to produce vitamin D.
Diet and supplements help fill the gap. While only a few foods naturally contain vitamin D, some are fortified to help meet daily needs. Here’s a quick look at some key dietary sources:
Supplements are another reliable way to maintain healthy vitamin D levels. They come in two forms: D2 (ergocalciferol), derived from plants, and D3 (cholecalciferol), which is naturally produced in your body and found in animal-based foods.
D3 is generally better at raising and maintaining blood vitamin D levels. For adults aged 19–70, the recommended daily intake is 600 IU (15 mcg), increasing to 800 IU (20 mcg) for those over 70. The upper safe limit is 4,000 IU (100 mcg) per day.
If you have minimal sun exposure or darker skin, a daily supplement of 1,000 to 2,000 IU might be a smart choice.
Vitamin D deficiency often sneaks in under the radar, disguising itself as everyday fatigue or stress. Many people chalk up their tiredness to the demands of daily life, unaware that their vitamin D levels might be dropping. These subtle and vague symptoms make it easy for a deficiency to go unnoticed.
Knowing what to watch for can help you catch this issue early, before it has a more serious impact on your health. Below, we’ll explore the key physical and mental warning signs, as well as the groups most at risk.
The symptoms of vitamin D deficiency can vary, but they often include fatigue, bone pain, and muscle issues. Fatigue is usually the first sign, but it’s easy to dismiss as a result of overworking or stress. Other physical symptoms include bone pain, muscle weakness, cramps, or general aches. These occur because vitamin D is essential for calcium absorption and muscle function.
Mental health can also take a hit. A deficiency in vitamin D has been linked to mood changes, including depression or persistent sadness. This makes sense, as vitamin D receptors are found throughout the brain and nervous system.
Interestingly, many people with vitamin D deficiency show no symptoms at all. If you’re dealing with unexplained fatigue and can’t pinpoint the cause—like illness or poor sleep—it might be worth getting your vitamin D levels tested.
Some groups are more likely to experience vitamin D deficiency due to factors like skin tone, age, lifestyle, or where they live. For example, people with darker skin are at a higher risk because melanin reduces the skin’s ability to produce vitamin D from sunlight.
Research shows that African-Americans need up to six times more UVB exposure than those with lighter skin to produce the same amount of vitamin D.
Age is another significant factor. Among seniors, deficiency rates range from 15% to 52%, with those in nursing homes being particularly vulnerable. In Sydney, for instance, 86% of women and 68% of men in nursing homes were found to have moderate deficiencies. Younger people aren’t immune either—17% of teenagers and 32% of young adults are deficient.
Geography and lifestyle also play a role. Urban areas report higher deficiency rates (27%) compared to inner regional (16%), outer regional (13%), and remote areas (9%). This urban-rural gap likely reflects differences in sun exposure and outdoor activities.
Certain ethnicities face higher risks too. For example, deficiency rates are high among individuals born in Southern and Central Asia (67%), Northeast Asia (64%), Southeast Asia (58%), and North Africa and the Middle East (50%).
Other high-risk groups include people who cover their skin for religious or cultural reasons, those with limited outdoor time due to work or lifestyle, and individuals with health conditions like obesity, PCOS, or insulin resistance. Interestingly, Australia’s "sun smart" campaign, while reducing sunburn rates, has also coincided with a rise in vitamin D deficiencies.
Regular checkups with a healthcare provider can help ensure your vitamin D levels are where they need to be—ideally before symptoms even start.
Looking to support your energy, mood, or cycle? Check out our guide to the best supplements for balancing hormones in Australia.
When your vitamin D levels dip, your body starts signalling trouble, often in ways that can range from subtle to serious. These issues can affect everything from your bones to your immune system.
Recognising the signs early can help you address potential problems before they escalate. Let’s take a closer look at how low vitamin D impacts different parts of the body.
Low vitamin D can affect your body right away or over time. Early signs include fatigue and low immunity, while long-term deficiency may lead to bone issues and chronic disease risk.
Your bones are the first to feel the effects of a vitamin D deficiency. Without enough vitamin D, your body struggles to absorb calcium effectively, setting off a chain reaction of bone-related issues. Even a mild, ongoing deficiency can lead to hypocalcaemia and secondary hyperparathyroidism, both of which increase the likelihood of osteoporosis, falls, and fractures.
In children, severe vitamin D deficiency can result in rickets, a condition characterised by abnormal growth, muscle weakness, bone pain, and joint deformities. For adults, the problem can progress to osteomalacia, where bones become soft and brittle, significantly raising the risk of fractures.
A lack of vitamin D can leave your immune system vulnerable, making you more prone to infections and autoimmune disorders.
Low vitamin D levels have been linked to a higher risk of cardiovascular disease and type 2 diabetes. Additionally, obesity increases the prevalence of vitamin D deficiency by 35%, creating a harmful cycle that’s tough to break.
Low levels of 25-hydroxyvitamin D are associated with a 30%–50% higher risk of developing colon, prostate, and breast cancers, along with increased cancer-related mortality.
Vitamin D deficiency has been connected to depression and mood disorders. Since vitamin D receptors are present throughout the brain and nervous system, insufficient levels may negatively affect mood, mental clarity, and overall cognitive health.
Understanding the severity of a deficiency can help guide appropriate treatment:
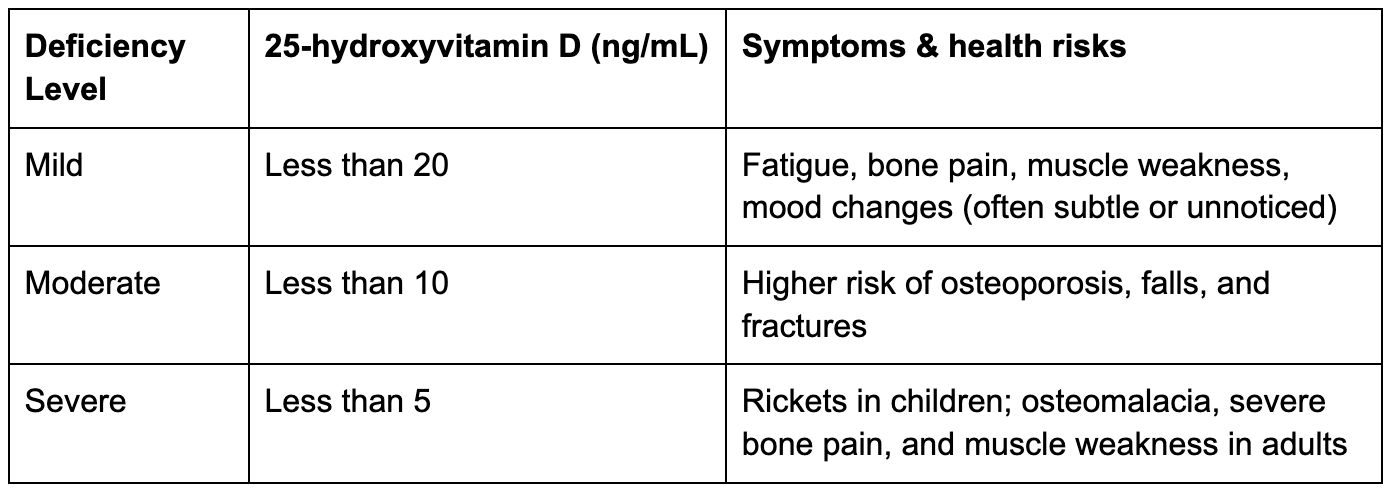
Mild deficiency can be easy to overlook. You might feel more tired than usual or have muscle aches that are mistaken for stress or overexertion. For children, even a mild deficiency might cause weak or sore muscles.
Severe deficiency, on the other hand, is much harder to ignore. Children may develop rickets, leading to visible bone deformities, while adults face osteomalacia with symptoms like soft, weak bones and significant pain. Older adults with vitamin D levels below 10 ng/mL are at a much greater risk of experiencing dangerous falls.
Addressing a deficiency early, whether mild or severe, can prevent these complications from becoming life-altering. Proper detection and treatment make all the difference.
Testing for vitamin D deficiency starts with recognising risk factors and symptoms. Knowing when to take this step can help catch potential problems early.
Doctors often recommend testing when patients report symptoms linked to vitamin D deficiency. These may include bone or muscle pain, increased sensitivity to pain, tingling sensations, muscle weakness, or a history of fractures.
Some medical conditions can interfere with how your body absorbs or processes vitamin D. These include cystic fibrosis, Crohn's disease, coeliac disease, obesity, kidney disease, and liver disease. If you have any of these, regular monitoring might be necessary.
Certain medications, like steroids, cholesterol-lowering drugs, seizure medications, rifampin, and orlistat, can reduce vitamin D levels over time. If you're on these medications, talk to your doctor about monitoring your levels.
Infants, especially those who are breastfed, and older adults, whose skin produces less vitamin D, are advised to undergo regular testing.
If you fall into any of these categories or are experiencing symptoms, the next step is to understand how to interpret your test results.
Curious about your cardiovascular fitness? Explore our complete guide to VO₂ max and how it connects to your long-term health goals.
Testing for vitamin D is straightforward. It typically involves a blood draw (or a finger prick/heel stick for infants), with results available within a few business days. No special preparation is required, though you should inform your doctor of any medications or supplements you’re taking.
Vitamin D levels are measured as 25-hydroxy concentrations in either nanomoles per liter (nmol/L) or nanograms per milliliter (ng/mL). Here's how the results are categorised:
What to ask your doctor
Once you have your results, discuss them with your healthcare provider. Key questions might include:
If your levels are low, your doctor may recommend dietary changes or supplements. On the other hand, if your levels are high, stop taking supplements immediately and consult your doctor.
Testing costs vary depending on the provider. Out-of-pocket expenses can range from $75 to $99, though many insurance plans cover the test if it’s medically necessary.
Want to learn how your habits are shaping your long-term health? Check out our guide on what your BioAge really means and how to improve it.
Once you’ve identified your vitamin D levels, it’s time to take steps to improve them. A combination of safe sun exposure, dietary adjustments, and supplements can help you get back on track.
Sunlight is the most natural way to boost vitamin D, but how much you need depends on factors like location, skin tone, and the time of year.
Where you live significantly impacts how much sunlight you need. For example, someone in Miami during the summer might only need 3 minutes of sun exposure with 25% of their skin exposed, while the same person would require 23 minutes at noon in Boston during winter. This explains why vitamin D deficiency is more common in northern states during the colder months.
Skin tone plays a big role in how much sun exposure is necessary. While 4–15 minutes of midday sun may work for lighter skin tones, individuals with darker skin need more time due to higher melanin levels, which naturally block UV rays and slow vitamin D production.
To safely benefit from the sun, expose your skin during midday when UVB rays are strongest. After 10–30 minutes of unprotected exposure, apply sunscreen to prevent burns. Keep in mind that UVB rays don’t penetrate glass, so sitting by a sunny window won’t help.
Interestingly, sunscreen doesn’t completely block UVB rays. Research shows that 15.6% of UV radiation still reaches the skin, even with sunscreen.
Beyond sunlight, you can turn to food and supplements to ensure your vitamin D levels stay optimal.
Since only a few foods naturally contain vitamin D, fatty fish is a great option. For instance, a 3.5-ounce serving of farmed Atlantic salmon provides 441 IU of vitamin D, while wild-caught salmon often offers even more.
Many everyday foods in Australia are fortified with vitamin D to make it easier to meet your needs. For example:
For plant-based eaters, UV-treated mushrooms are a fantastic source of vitamin D. A single cup of cremini mushrooms exposed to UV light packs 1,100 IU of vitamin D - 139% of the daily value. These mushrooms are becoming more widely available in grocery stores.
If food and sunlight aren’t enough, supplements can fill the gap. Vitamin D3 (cholecalciferol) is more effective than D2 at raising blood vitamin D levels. The recommended daily allowance varies by age:
Look for third-party tested supplements to ensure quality.
For a more comprehensive approach, consider combining these strategies with tools that monitor your overall health.
Addressing vitamin D deficiency isn’t just about bone health—it also supports your metabolism. Vitamin D plays a role in how your body processes nutrients and maintains energy balance. This makes it a great time to adopt a holistic approach by tracking other aspects of your health.
Health tracking tools can show how improving vitamin D levels impacts your overall metabolic health. Platforms like Vively, which offer continuous glucose monitoring (CGM), let you see real-time data on how dietary changes like adding vitamin D-rich foods or supplements affect your glucose levels and metabolic function.
The lifestyle changes that help with vitamin D deficiency, like midday sun exposure, eating nutrient-packed foods, and sticking to a supplement routine, often benefit your metabolism as well. By using health monitoring tools, you can track how these changes positively influence your overall health.
When you’re already working on improving your vitamin D levels, it’s the perfect time to implement other health strategies. With continuous monitoring, you can identify which dietary choices work best for your body, optimising both your vitamin D levels and your metabolic health.
Managing your vitamin D levels through sunlight, food, and supplements is a great step, but it also helps to see how these changes fit into your bigger health picture. Vively gives you real-time insights into your metabolic health so you can make informed decisions every day.
With Vively, you can:
Vitamin D affects more than bone health—it also plays a role in metabolism and energy regulation. Vively helps you stay in tune with your body and create habits that truly support your wellbeing.
Vitamin D deficiency affects a large portion of the population. By combining safe sun exposure, a nutrient-packed diet, and supplements, you can take control of your vitamin D levels and support overall health.
Try to get 15–30 minutes of sun exposure a few times a week, include foods like fatty fish and fortified products in your meals, and consider adding vitamin D₃ supplements to your routine.
Your specific needs depend on factors like your skin tone, age, location, and daily habits. The Endocrine Society suggests most healthy adults aim for 1,500 to 2,000 IU per day, but consulting a healthcare provider is the best way to tailor this to your situation.
The encouraging part? Vitamin D deficiency is manageable with the right approach. For better absorption, take your vitamin D supplements with meals that include healthy fats. Additionally, tools like continuous glucose monitors can offer insights into how optimising vitamin D levels benefits your overall metabolic health.
Taking steps to balance your vitamin D levels now can lead to stronger bones, a healthier immune system, and better metabolic well-being.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
