Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan




Anti-Müllerian Hormone (AMH) is a key fertility marker that reflects your ovarian reserve - essentially, the number of eggs you have left. An AMH blood test offers consistent results regardless of your menstrual cycle, making it a dependable tool for fertility planning. However, AMH measures egg quantity, not quality, and should be interpreted alongside other factors like age and overall health.
Key takeaways:
If you’re planning for pregnancy, AMH testing can guide your decisions, but it’s just one piece of the puzzle. Always consult a healthcare provider for a full fertility evaluation.
The AMH test is a simple and convenient procedure. A healthcare provider draws a small blood sample from a vein in your arm, which is quick and doesn’t require any special preparation. One of the key benefits of the AMH test is its flexibility; you can take it at any point during your menstrual cycle, as AMH levels stay relatively consistent throughout.
There’s no need to fast or modify your diet before the test. However, it’s important to inform your healthcare provider about any medications you’re taking, as some can influence AMH levels. Also, mention any recent changes in your health that might affect the test results.
Once the blood sample is drawn, it’s sent to a lab for analysis, with results typically available in a few days. Your healthcare provider will then review the findings with you, explaining what they mean in the context of your overall health and fertility. The results offer valuable information about your ovarian reserve.
AMH levels, measured in nanograms per milliliter (ng/mL), provide insight into the number of eggs remaining in your ovaries. Higher AMH levels indicate a larger egg supply, while lower levels suggest a diminished reserve.
Here’s a general breakdown of AMH ranges:
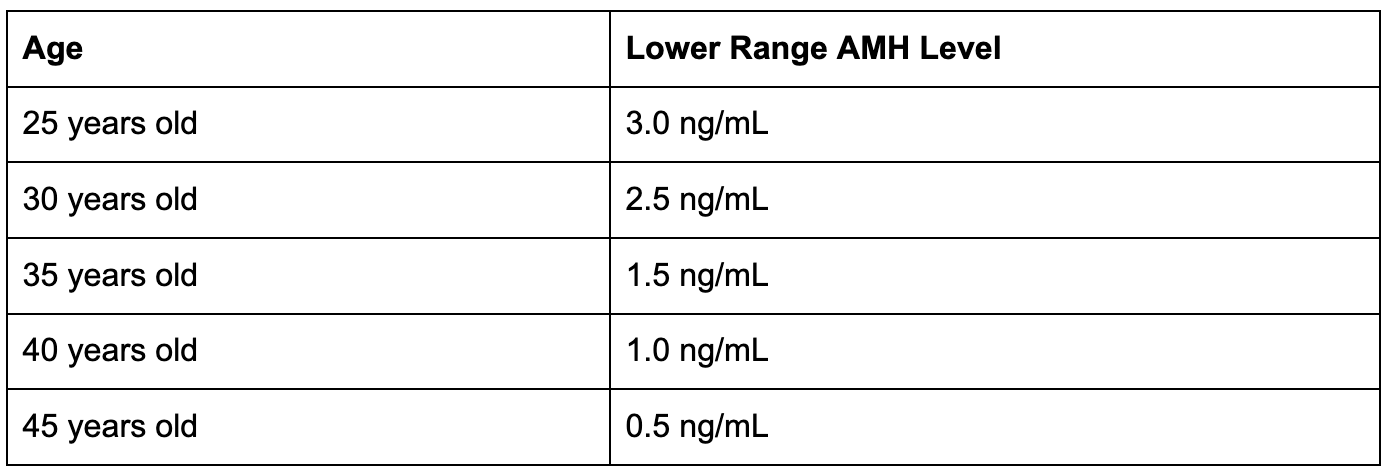
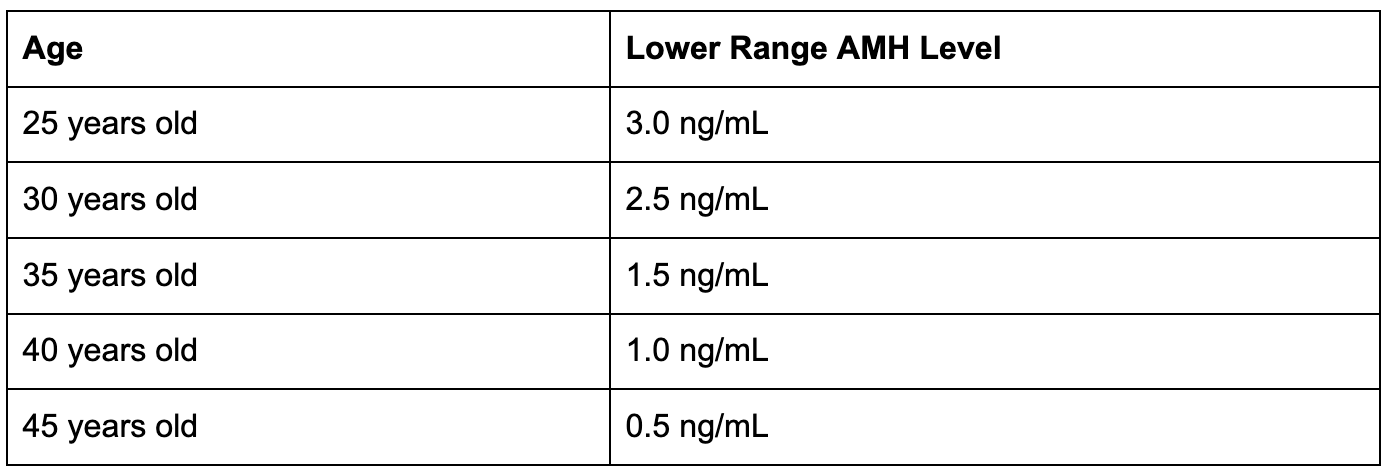
Age plays a critical role in interpreting these numbers, as AMH levels naturally decline over time. Below is a table showing estimated lower-range AMH levels by age:
The AMH test also helps predict ovarian response to injectable fertility medications used in IVF.
Interpreting AMH levels requires a specialist who can assess them alongside other factors in a broader fertility evaluation. The numbers alone don’t provide a complete picture of your fertility potential.
Several factors can influence AMH levels, beyond just the test results. Age remains the most significant factor in determining fertility outcomes, as AMH levels naturally decline with age. Research shows a clear negative correlation between age and AMH levels in adult women.
Other influences include:
It’s also worth noting that AMH levels can naturally fluctuate, so a single test might not fully capture your ovarian reserve. This variability highlights the importance of interpreting AMH levels within the broader context of your overall health and hormonal environment. Your healthcare provider will take all these factors into account when discussing your results.
Your Anti-Müllerian Hormone (AMH) level provides insight into your ovarian reserve, helping you plan for pregnancy based on your age and personal goals. If your AMH level is below 1.0 ng/mL, it may suggest a reduced ovarian reserve. For women over 35, this could mean it’s better to start trying for a baby sooner rather than later.
Research shows natural conception rates vary by AMH levels: 11.2% for low AMH, 14.3% for normal, and 15.7% for high AMH. However, younger women under 35 with low AMH levels often maintain fertility comparable to their peers.
AMH levels also play a role in decisions about egg freezing. They help predict how many eggs might be retrieved in a cycle. For example, women aged 34 or younger typically freeze around 17 eggs per cycle, while women over 41 retrieve fewer than 10 eggs on average.
A 2017 study in Human Reproduction found that women aged 41 or older would need to freeze 20 eggs to have a 50% chance of a live birth, compared to just 7 eggs for women aged 34 or younger.
Understanding whether your AMH level is high or low can guide your family planning approach. Low AMH levels generally indicate fewer available eggs. While this doesn’t eliminate the possibility of natural conception, it may reduce the number of eggs retrieved during IVF. Interestingly, studies show that younger women with low AMH levels can achieve IVF success rates similar to those with normal AMH levels.
Additionally, lifestyle changes like regular low-impact exercise, cutting back on alcohol and caffeine, quitting smoking, and taking high-quality vitamins may improve IVF outcomes. Complementary practices like acupuncture or massage can also be beneficial.
High AMH levels usually signal a larger egg reserve. However, levels above 4.0 ng/mL may indicate polycystic ovary syndrome (PCOS), which can require specialized fertility treatments.
In IVF, high AMH levels are linked to better outcomes, such as higher live birth rates, more eggs retrieved, and better chances for embryo freezing. However, extremely high levels (above 5 ng/mL) can increase the risk of ovarian hyperstimulation syndrome (OHSS), which may lead to complications. Research shows that for every 1 ng/mL increase in AMH above 5 ng/mL, the odds of a live birth drop by 3% due to fresh embryo transfer cancellations.
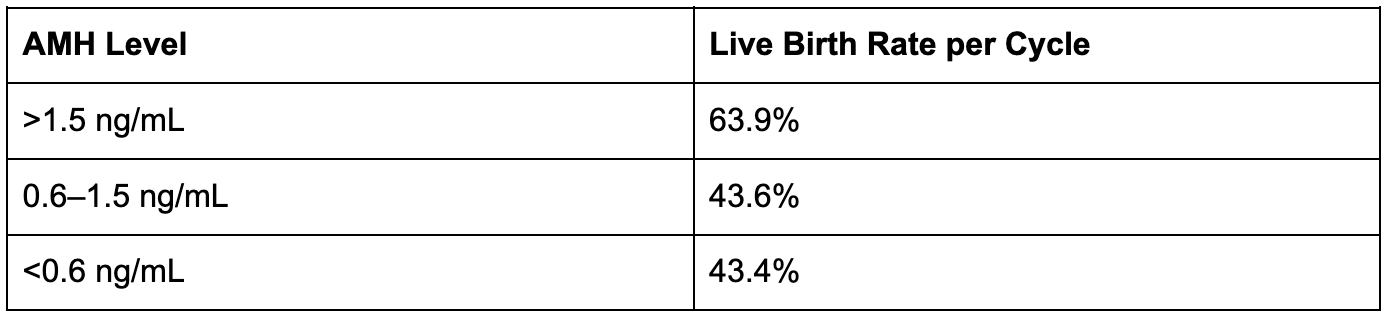
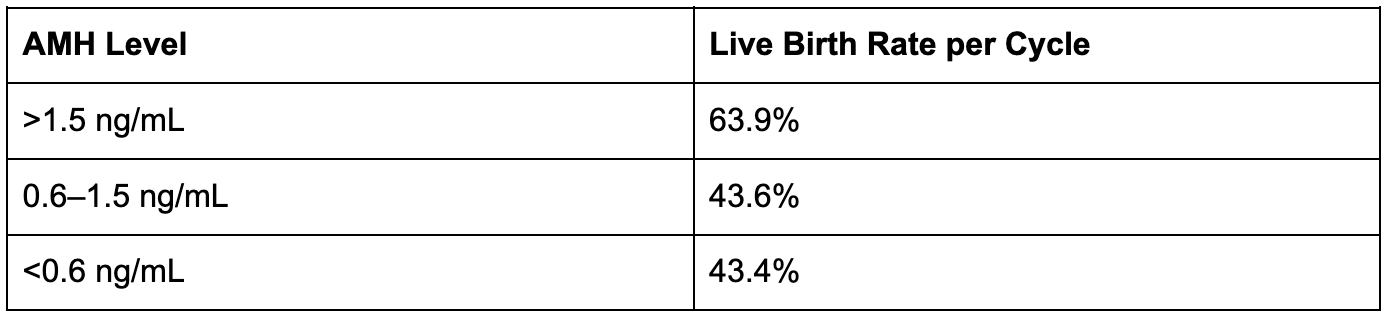
Here’s a quick look at how AMH levels affect IVF outcomes for women under 35:
1. Myth: AMH alone determines your fertility success.
While AMH provides an estimate of ovarian reserve, it doesn’t fully predict fertility.
2. Myth: Low AMH means you can't get pregnant naturally.
Even with low AMH, many women conceive naturally. For younger women, AMH levels are more about egg quantity than quality.
3. Myth: High AMH guarantees easy conception.
While high AMH reflects a larger egg supply, it doesn’t always make conception easier. Very high levels are often linked to PCOS, which can complicate ovulation and natural conception.
4. Myth: AMH testing should cause fertility anxiety.
AMH testing is just one part of a broader fertility assessment. It’s a tool to guide planning, not a definitive measure of your reproductive future. Research highlights the importance of avoiding unnecessary stress, particularly for younger women with lower AMH levels.
Could tracking your glucose help you better understand how your body responds during fertility planning? Learn more in our guide on the diverse applications of CGM in women’s health.
Pairing AMH testing with other fertility assessments can provide a clearer picture of reproductive health. Since egg count naturally decreases over time, combining multiple tests helps improve accuracy.
One common test used alongside AMH is the Antral Follicle Count (AFC). This involves a pelvic ultrasound where your doctor counts the small follicles in your ovaries. These follicles are an indicator of your remaining egg supply. When AFC results are combined with AMH levels, the assessment of ovarian reserve becomes more precise.
Another important test is Follicle-Stimulating Hormone (FSH) measurement. FSH is responsible for stimulating egg development. Unlike AMH, which remains stable throughout the menstrual cycle, FSH must be tested on cycle days 2 to 5. Elevated FSH levels may suggest reduced ovarian function, while normal levels indicate a healthy response.
Estradiol testing is often done alongside FSH to provide additional insights into ovarian function. Together, these tests evaluate whether your ovaries are responding properly to hormonal signals.
For male partners, a semen analysis evaluates sperm count, movement, and shape, offering crucial information about male fertility potential.
Beyond testing, there are lifestyle changes and medical options that can help improve fertility outcomes.
While AMH levels are primarily influenced by age and genetics, there are steps you can take to optimize reproductive health. A combination of lifestyle adjustments and medical treatments can make a meaningful difference.
Dietary choices are key. A Mediterranean-style diet rich in omega-3 fatty acids, antioxidants, and vitamin D has been linked to better egg quality and ovarian function. Supplements like Coenzyme Q10 may also support fertility.
Exercise and stress management can improve hormonal balance. Moderate physical activity and stress-relieving practices like yoga or meditation are beneficial for overall fertility.
Environmental factors should not be overlooked. Avoiding smoking and limiting alcohol consumption can help protect egg quality. Reducing exposure to environmental toxins, such as BPA, by using natural cleaning products and BPA-free plastics, may also be helpful.
Certain factors, like autoimmune conditions, surgeries for ovarian cysts or endometriosis, and high biotin intake, can lower AMH levels. While genetic factors cannot be changed, addressing modifiable risks, such as quitting smoking or managing environmental exposures - can support fertility potential.
When lifestyle changes alone are not enough, medical treatments can be an option. For women with PCOS-related infertility, letrozole is now the preferred oral medication for inducing ovulation, with clomiphene citrate serving as an alternative. However, clomiphene resistance occurs in about 25% of women with PCOS-related infertility.
If AMH results indicate a low ovarian reserve, it’s essential to discuss options with your healthcare provider. These may include trying to conceive sooner, using donor eggs if appropriate, or considering egg freezing for the future.
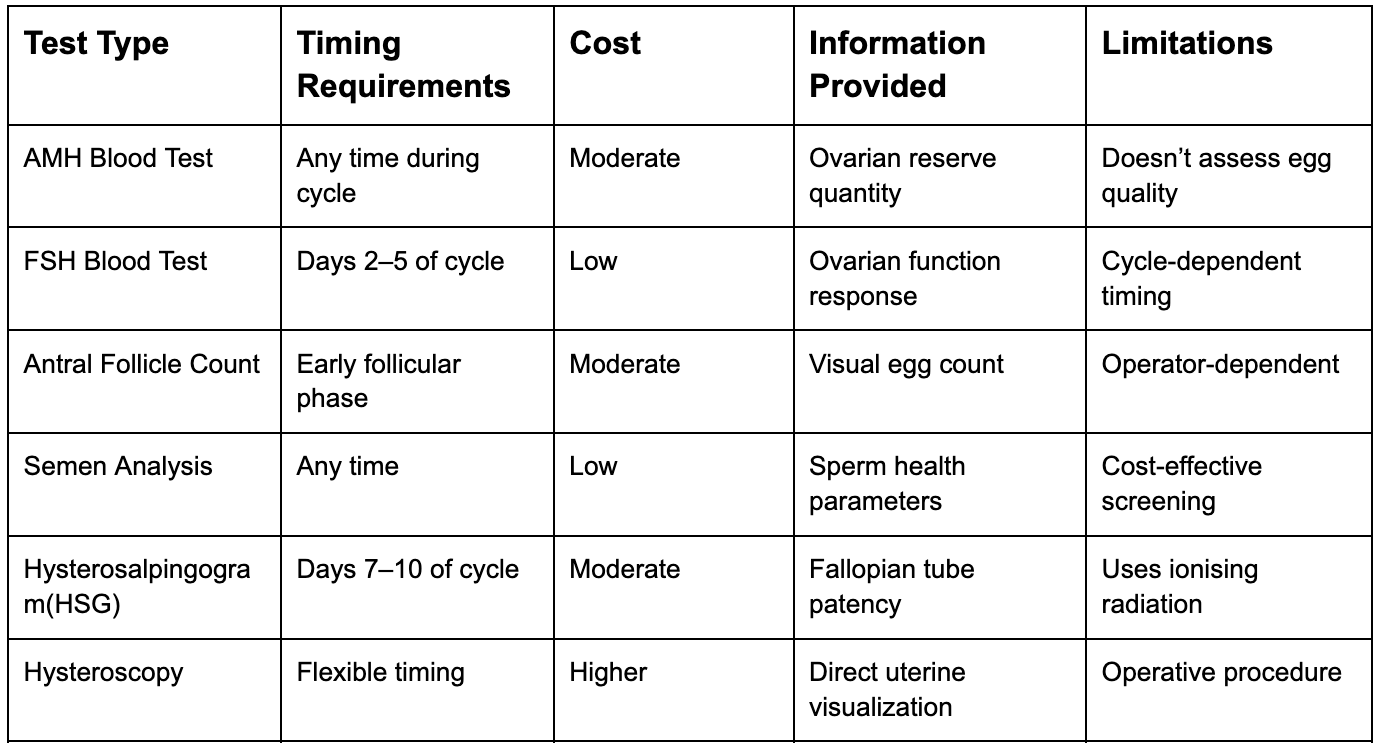
To help you choose the right fertility tests, here’s a comparison of key tools, outlining their timing, costs, and benefits:
At-home fertility tests offer convenience for initial screenings, such as checking ovulation timing or basic semen parameters. However, they can’t replace the detailed evaluations performed by specialists.
In-office testing provides more specific insights into infertility causes, enabling tailored treatment plans. Simple methods like basal body temperature charting are cost-effective for tracking ovulation, while urinary LH kits help with timing diagnostic procedures and intercourse.
Advanced imaging techniques, like sonohysterography, have improved ultrasonography’s ability to diagnose infertility. Often combined with hysteroscopy, these methods provide alternatives to tests that use ionising radiation.
Most infertility evaluations can be completed within a few menstrual cycles, and some insurance plans may cover the costs. Be sure to check with your provider to understand your coverage and any out-of-pocket expenses.
Working closely with your healthcare provider is essential to developing a personalised assessment plan that aligns with your reproductive goals and lifestyle.
Your metabolism plays a pivotal role in reproductive health, influencing everything from hormone balance to the quality of eggs and sperm. When metabolic hormones like insulin, leptin, and ghrelin are out of sync, they can disrupt the regulation of reproductive hormones, creating challenges for fertility.
Obesity significantly increases the risk of infertility. In fact, each BMI unit above 29 kg/m² lowers the likelihood of pregnancy by 5%. This connection impacts both men and women. For men, studies reveal that metabolic health directly affects testosterone levels and sperm quality, including concentration and motility. In women, obesity can lead to ovulation problems and, in severe cases, permanent infertility.
Insulin resistance adds another layer of complexity, particularly for women with polycystic ovary syndrome (PCOS). This condition affects 50–70% of women with PCOS and is often accompanied by metabolic syndrome, hypertension, and diabetes.
Metabolic disorders can also trigger oxidative stress, an imbalance between harmful pro-oxidants and protective antioxidants. This stress may lead to reproductive challenges and even unexplained infertility.
The good news? A healthy metabolism achieved through a balanced diet, lifestyle changes, and weight management can help regulate hormones and promote ovulation. These insights are paving the way for advanced tools and strategies to enhance fertility outcomes.
Continuous glucose monitoring (CGM) offers a powerful way to connect metabolic health to fertility outcomes. By providing real-time data, CGM helps you understand how daily habits like diet, exercise, sleep, and stress impact your glucose levels and overall metabolic health. Programs like Vively’s CGM system make it easier to identify patterns and make informed decisions.
This technology is particularly valuable for uncovering metabolic issues that standard tests might miss. For instance, women with PCOS often experience unusual glucose spikes after meals, which underlines the importance of continuous monitoring. Considering that PCOS affects up to 20% of women in developed countries, stabilising insights is critical.
Maintaining steady glucose levels can improve energy, stabilise the nervous system, support weight management, and enhance fertilisation in men; keeping glucose levels in check is essential for sperm motility and fertilisation. CGM helps pinpoint which foods and lifestyle choices lead to glucose imbalances, enabling better decisions for reproductive health.
CGM devices offer immediate feedback, transforming how individuals prepare for pregnancy. This real-time approach allows for quicker adjustments to diet, exercise, and other lifestyle factors, improving overall metabolic health.
Metrics like time-in-range (TIR) provide practical targets. Research shows that even a 5% increase in TIR can lead to meaningful health benefits. For pregnancy preparation, a TIR goal of over 70%, equivalent to more than 16 hours and 48 minutes daily with stable glucose levels can be highly effective. Additionally, it’s important to keep time above range (TAR) under 25% (less than 6 hours per day) and time below range (TBR) under 4% (less than 1 hour per day with glucose levels below 63 mg/dL).
Regular CGM use, ideally active at least 70% of the time, helps identify patterns related to stress, sleep, exercise, and diet that might otherwise go unnoticed. Studies show that pregnant women using CGM experience a 0.19% lower mean HbA1c compared to non-users and spend more time in the target glucose range (68% with CGM versus 61% without).
Knowing your AMH levels is an important step in understanding your fertility, but it’s just one part of the bigger picture. Your reproductive health is closely linked to your overall metabolic health, which can influence hormone balance, ovulation, and pregnancy outcomes. Vively’s continuous glucose monitoring (CGM) program can support you by:

By pairing your AMH insights with Vively’s metabolic tracking, you gain a clearer understanding of how your daily habits impact your fertility and can take proactive steps toward a healthy pregnancy.
AMH testing gives insight into the number of growing follicles in your ovaries, offering a snapshot of your functional ovarian reserve. Studies indicate that AMH is a more reliable indicator of ovarian reserve compared to factors like age, BMI, or FSH levels alone.
This test is particularly useful for fertility planning. It helps guide decisions about treatments such as IVF, egg freezing, and medication dosages. Comparing your AMH levels with others in your age group can also provide additional context about your reproductive health.
That said, AMH is just one factor in the broader picture of fertility.
While AMH is a helpful tool, fertility outcomes are influenced by a wide range of factors, including metabolic health, age, lifestyle, and even your partner's health. This comprehensive approach is especially important considering that infertility affects about 1 in 6 people globally.
Maintaining steady glucose levels, often tracked with a CGM, can support hormonal balance, which is vital for fertility. Conditions like polycystic ovary syndrome (PCOS), which AMH testing can help identify, are frequently tied to metabolic challenges.
If your AMH levels are on the lower side, early action can be crucial. Fertility specialists may recommend trying to conceive sooner or exploring options like egg freezing. Combining your AMH results with a full understanding of your overall health can greatly enhance your chances of reaching your pregnancy goals.
AMH testing plays an important role in evaluating ovarian reserve, giving insight into how many eggs are left in the ovaries. This can be a key piece of the puzzle when it comes to understanding fertility and planning for pregnancy.
To get a fuller picture of fertility health, AMH testing is often combined with other evaluations, such as:
By combining these assessments, you and your healthcare provider can gain a deeper understanding of your fertility and make more informed choices about your family planning goals.
When it comes to Anti-Müllerian Hormone (AMH) levels, age and genetics are the primary factors at play. However, adopting healthier habits can still make a difference in your overall fertility. Eating a nutrient-rich diet filled with antioxidants, vitamins, and healthy fats, paired with consistent moderate exercise, may help support ovarian health and boost reproductive well-being.
In contrast, certain lifestyle choices like smoking, heavy drinking, or dealing with prolonged stress can take a toll on fertility. While these changes might not significantly shift AMH levels, they can contribute to better reproductive health and improve your chances of conceiving.
High Anti-Müllerian Hormone (AMH) levels are frequently associated with polycystic ovary syndrome (PCOS), a condition that disrupts hormone levels and affects ovulation. Elevated AMH usually indicates a higher number of ovarian follicles, which is a hallmark of PCOS.
While having more follicles might sound like a positive sign for fertility, it can actually interfere with ovulation. In cases of PCOS, these follicles often fail to release mature eggs, which can make natural conception more challenging. If you’re dealing with irregular menstrual cycles or struggling to conceive, it’s worth consulting a healthcare provider to explore whether high AMH levels or PCOS could be playing a role.
How does AMH testing contribute to understanding fertility, and what other evaluations should I consider?
AMH testing plays an important role in evaluating ovarian reserve, giving insight into how many eggs are left in the ovaries. This can be a key piece of the puzzle when it comes to understanding fertility and planning for pregnancy.
To get a fuller picture of fertility health, AMH testing is often combined with other evaluations, such as:
By combining these assessments, you and your healthcare provider can gain a deeper understanding of your fertility and make more informed choices about your family planning goals.
When it comes to Anti-Müllerian Hormone (AMH) levels, age and genetics are the primary factors at play. However, adopting healthier habits can still make a difference in your overall fertility. Eating a nutrient-rich diet filled with antioxidants, vitamins, and healthy fats, paired with consistent moderate exercise, may help support ovarian health and boost reproductive well-being.
In contrast, certain lifestyle choices like smoking, heavy drinking, or dealing with prolonged stress can take a toll on fertility. While these changes might not significantly shift AMH levels, they can contribute to better reproductive health and improve your chances of conceiving.
High Anti-Müllerian Hormone (AMH) levels are frequently associated with polycystic ovary syndrome (PCOS), a condition that disrupts hormone levels and affects ovulation. Elevated AMH usually indicates a higher number of ovarian follicles, which is a hallmark of PCOS.
While having more follicles might sound like a positive sign for fertility, it can actually interfere with ovulation. In cases of PCOS, these follicles often fail to release mature eggs, which can make natural conception more challenging. If you’re dealing with irregular menstrual cycles or struggling to conceive, it’s worth consulting a healthcare provider to explore whether high AMH levels or PCOS could be playing a role.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Anti-Müllerian Hormone (AMH) is a key fertility marker that reflects your ovarian reserve - essentially, the number of eggs you have left. An AMH blood test offers consistent results regardless of your menstrual cycle, making it a dependable tool for fertility planning. However, AMH measures egg quantity, not quality, and should be interpreted alongside other factors like age and overall health.
Key takeaways:
If you’re planning for pregnancy, AMH testing can guide your decisions, but it’s just one piece of the puzzle. Always consult a healthcare provider for a full fertility evaluation.
The AMH test is a simple and convenient procedure. A healthcare provider draws a small blood sample from a vein in your arm, which is quick and doesn’t require any special preparation. One of the key benefits of the AMH test is its flexibility; you can take it at any point during your menstrual cycle, as AMH levels stay relatively consistent throughout.
There’s no need to fast or modify your diet before the test. However, it’s important to inform your healthcare provider about any medications you’re taking, as some can influence AMH levels. Also, mention any recent changes in your health that might affect the test results.
Once the blood sample is drawn, it’s sent to a lab for analysis, with results typically available in a few days. Your healthcare provider will then review the findings with you, explaining what they mean in the context of your overall health and fertility. The results offer valuable information about your ovarian reserve.
AMH levels, measured in nanograms per milliliter (ng/mL), provide insight into the number of eggs remaining in your ovaries. Higher AMH levels indicate a larger egg supply, while lower levels suggest a diminished reserve.
Here’s a general breakdown of AMH ranges:
Age plays a critical role in interpreting these numbers, as AMH levels naturally decline over time. Below is a table showing estimated lower-range AMH levels by age:
The AMH test also helps predict ovarian response to injectable fertility medications used in IVF.
Interpreting AMH levels requires a specialist who can assess them alongside other factors in a broader fertility evaluation. The numbers alone don’t provide a complete picture of your fertility potential.
Several factors can influence AMH levels, beyond just the test results. Age remains the most significant factor in determining fertility outcomes, as AMH levels naturally decline with age. Research shows a clear negative correlation between age and AMH levels in adult women.
Other influences include:
It’s also worth noting that AMH levels can naturally fluctuate, so a single test might not fully capture your ovarian reserve. This variability highlights the importance of interpreting AMH levels within the broader context of your overall health and hormonal environment. Your healthcare provider will take all these factors into account when discussing your results.
Your Anti-Müllerian Hormone (AMH) level provides insight into your ovarian reserve, helping you plan for pregnancy based on your age and personal goals. If your AMH level is below 1.0 ng/mL, it may suggest a reduced ovarian reserve. For women over 35, this could mean it’s better to start trying for a baby sooner rather than later.
Research shows natural conception rates vary by AMH levels: 11.2% for low AMH, 14.3% for normal, and 15.7% for high AMH. However, younger women under 35 with low AMH levels often maintain fertility comparable to their peers.
AMH levels also play a role in decisions about egg freezing. They help predict how many eggs might be retrieved in a cycle. For example, women aged 34 or younger typically freeze around 17 eggs per cycle, while women over 41 retrieve fewer than 10 eggs on average.
A 2017 study in Human Reproduction found that women aged 41 or older would need to freeze 20 eggs to have a 50% chance of a live birth, compared to just 7 eggs for women aged 34 or younger.
Understanding whether your AMH level is high or low can guide your family planning approach. Low AMH levels generally indicate fewer available eggs. While this doesn’t eliminate the possibility of natural conception, it may reduce the number of eggs retrieved during IVF. Interestingly, studies show that younger women with low AMH levels can achieve IVF success rates similar to those with normal AMH levels.
Additionally, lifestyle changes like regular low-impact exercise, cutting back on alcohol and caffeine, quitting smoking, and taking high-quality vitamins may improve IVF outcomes. Complementary practices like acupuncture or massage can also be beneficial.
High AMH levels usually signal a larger egg reserve. However, levels above 4.0 ng/mL may indicate polycystic ovary syndrome (PCOS), which can require specialized fertility treatments.
In IVF, high AMH levels are linked to better outcomes, such as higher live birth rates, more eggs retrieved, and better chances for embryo freezing. However, extremely high levels (above 5 ng/mL) can increase the risk of ovarian hyperstimulation syndrome (OHSS), which may lead to complications. Research shows that for every 1 ng/mL increase in AMH above 5 ng/mL, the odds of a live birth drop by 3% due to fresh embryo transfer cancellations.
Here’s a quick look at how AMH levels affect IVF outcomes for women under 35:
1. Myth: AMH alone determines your fertility success.
While AMH provides an estimate of ovarian reserve, it doesn’t fully predict fertility.
2. Myth: Low AMH means you can't get pregnant naturally.
Even with low AMH, many women conceive naturally. For younger women, AMH levels are more about egg quantity than quality.
3. Myth: High AMH guarantees easy conception.
While high AMH reflects a larger egg supply, it doesn’t always make conception easier. Very high levels are often linked to PCOS, which can complicate ovulation and natural conception.
4. Myth: AMH testing should cause fertility anxiety.
AMH testing is just one part of a broader fertility assessment. It’s a tool to guide planning, not a definitive measure of your reproductive future. Research highlights the importance of avoiding unnecessary stress, particularly for younger women with lower AMH levels.
Could tracking your glucose help you better understand how your body responds during fertility planning? Learn more in our guide on the diverse applications of CGM in women’s health.
Pairing AMH testing with other fertility assessments can provide a clearer picture of reproductive health. Since egg count naturally decreases over time, combining multiple tests helps improve accuracy.
One common test used alongside AMH is the Antral Follicle Count (AFC). This involves a pelvic ultrasound where your doctor counts the small follicles in your ovaries. These follicles are an indicator of your remaining egg supply. When AFC results are combined with AMH levels, the assessment of ovarian reserve becomes more precise.
Another important test is Follicle-Stimulating Hormone (FSH) measurement. FSH is responsible for stimulating egg development. Unlike AMH, which remains stable throughout the menstrual cycle, FSH must be tested on cycle days 2 to 5. Elevated FSH levels may suggest reduced ovarian function, while normal levels indicate a healthy response.
Estradiol testing is often done alongside FSH to provide additional insights into ovarian function. Together, these tests evaluate whether your ovaries are responding properly to hormonal signals.
For male partners, a semen analysis evaluates sperm count, movement, and shape, offering crucial information about male fertility potential.
Beyond testing, there are lifestyle changes and medical options that can help improve fertility outcomes.
While AMH levels are primarily influenced by age and genetics, there are steps you can take to optimize reproductive health. A combination of lifestyle adjustments and medical treatments can make a meaningful difference.
Dietary choices are key. A Mediterranean-style diet rich in omega-3 fatty acids, antioxidants, and vitamin D has been linked to better egg quality and ovarian function. Supplements like Coenzyme Q10 may also support fertility.
Exercise and stress management can improve hormonal balance. Moderate physical activity and stress-relieving practices like yoga or meditation are beneficial for overall fertility.
Environmental factors should not be overlooked. Avoiding smoking and limiting alcohol consumption can help protect egg quality. Reducing exposure to environmental toxins, such as BPA, by using natural cleaning products and BPA-free plastics, may also be helpful.
Certain factors, like autoimmune conditions, surgeries for ovarian cysts or endometriosis, and high biotin intake, can lower AMH levels. While genetic factors cannot be changed, addressing modifiable risks, such as quitting smoking or managing environmental exposures - can support fertility potential.
When lifestyle changes alone are not enough, medical treatments can be an option. For women with PCOS-related infertility, letrozole is now the preferred oral medication for inducing ovulation, with clomiphene citrate serving as an alternative. However, clomiphene resistance occurs in about 25% of women with PCOS-related infertility.
If AMH results indicate a low ovarian reserve, it’s essential to discuss options with your healthcare provider. These may include trying to conceive sooner, using donor eggs if appropriate, or considering egg freezing for the future.
To help you choose the right fertility tests, here’s a comparison of key tools, outlining their timing, costs, and benefits:
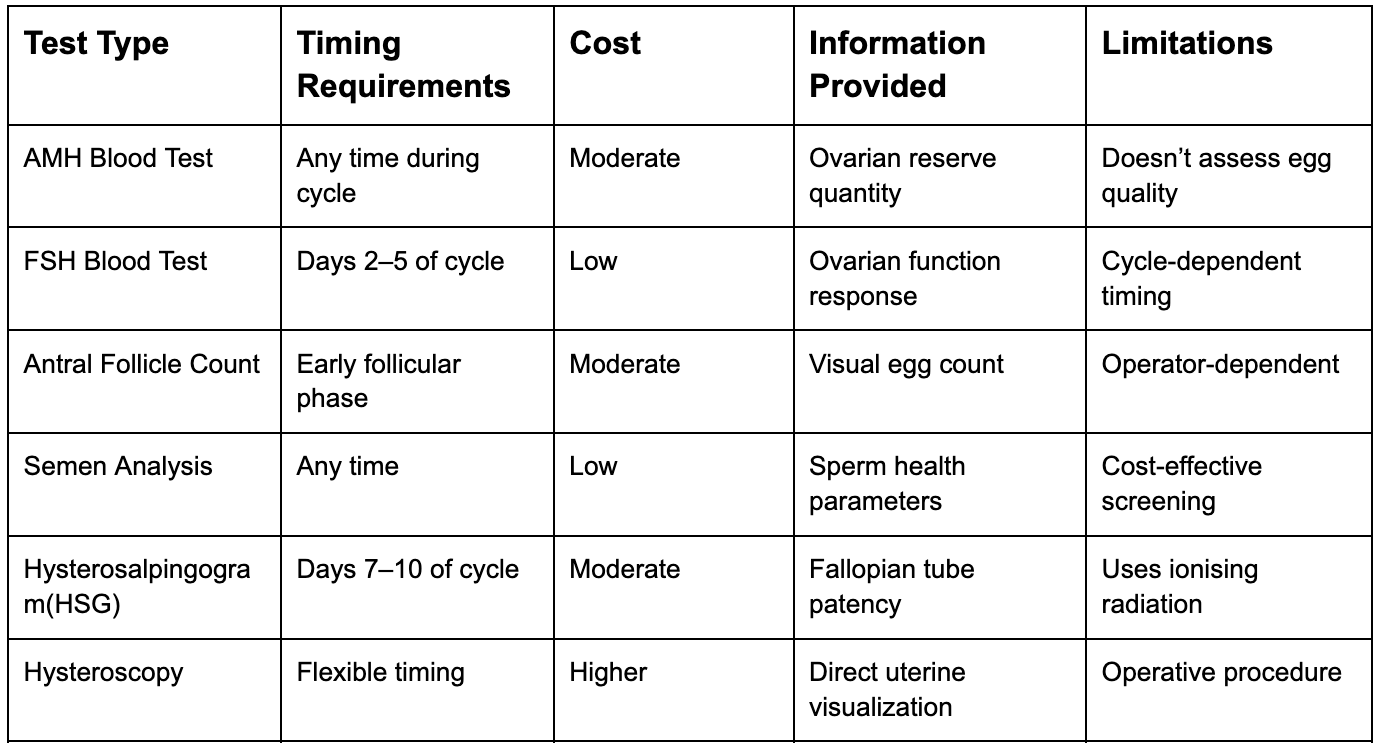
At-home fertility tests offer convenience for initial screenings, such as checking ovulation timing or basic semen parameters. However, they can’t replace the detailed evaluations performed by specialists.
In-office testing provides more specific insights into infertility causes, enabling tailored treatment plans. Simple methods like basal body temperature charting are cost-effective for tracking ovulation, while urinary LH kits help with timing diagnostic procedures and intercourse.
Advanced imaging techniques, like sonohysterography, have improved ultrasonography’s ability to diagnose infertility. Often combined with hysteroscopy, these methods provide alternatives to tests that use ionising radiation.
Most infertility evaluations can be completed within a few menstrual cycles, and some insurance plans may cover the costs. Be sure to check with your provider to understand your coverage and any out-of-pocket expenses.
Working closely with your healthcare provider is essential to developing a personalised assessment plan that aligns with your reproductive goals and lifestyle.
Your metabolism plays a pivotal role in reproductive health, influencing everything from hormone balance to the quality of eggs and sperm. When metabolic hormones like insulin, leptin, and ghrelin are out of sync, they can disrupt the regulation of reproductive hormones, creating challenges for fertility.
Obesity significantly increases the risk of infertility. In fact, each BMI unit above 29 kg/m² lowers the likelihood of pregnancy by 5%. This connection impacts both men and women. For men, studies reveal that metabolic health directly affects testosterone levels and sperm quality, including concentration and motility. In women, obesity can lead to ovulation problems and, in severe cases, permanent infertility.
Insulin resistance adds another layer of complexity, particularly for women with polycystic ovary syndrome (PCOS). This condition affects 50–70% of women with PCOS and is often accompanied by metabolic syndrome, hypertension, and diabetes.
Metabolic disorders can also trigger oxidative stress, an imbalance between harmful pro-oxidants and protective antioxidants. This stress may lead to reproductive challenges and even unexplained infertility.
The good news? A healthy metabolism achieved through a balanced diet, lifestyle changes, and weight management can help regulate hormones and promote ovulation. These insights are paving the way for advanced tools and strategies to enhance fertility outcomes.
Continuous glucose monitoring (CGM) offers a powerful way to connect metabolic health to fertility outcomes. By providing real-time data, CGM helps you understand how daily habits like diet, exercise, sleep, and stress impact your glucose levels and overall metabolic health. Programs like Vively’s CGM system make it easier to identify patterns and make informed decisions.
This technology is particularly valuable for uncovering metabolic issues that standard tests might miss. For instance, women with PCOS often experience unusual glucose spikes after meals, which underlines the importance of continuous monitoring. Considering that PCOS affects up to 20% of women in developed countries, stabilising insights is critical.
Maintaining steady glucose levels can improve energy, stabilise the nervous system, support weight management, and enhance fertilisation in men; keeping glucose levels in check is essential for sperm motility and fertilisation. CGM helps pinpoint which foods and lifestyle choices lead to glucose imbalances, enabling better decisions for reproductive health.
CGM devices offer immediate feedback, transforming how individuals prepare for pregnancy. This real-time approach allows for quicker adjustments to diet, exercise, and other lifestyle factors, improving overall metabolic health.
Metrics like time-in-range (TIR) provide practical targets. Research shows that even a 5% increase in TIR can lead to meaningful health benefits. For pregnancy preparation, a TIR goal of over 70%, equivalent to more than 16 hours and 48 minutes daily with stable glucose levels can be highly effective. Additionally, it’s important to keep time above range (TAR) under 25% (less than 6 hours per day) and time below range (TBR) under 4% (less than 1 hour per day with glucose levels below 63 mg/dL).
Regular CGM use, ideally active at least 70% of the time, helps identify patterns related to stress, sleep, exercise, and diet that might otherwise go unnoticed. Studies show that pregnant women using CGM experience a 0.19% lower mean HbA1c compared to non-users and spend more time in the target glucose range (68% with CGM versus 61% without).
Knowing your AMH levels is an important step in understanding your fertility, but it’s just one part of the bigger picture. Your reproductive health is closely linked to your overall metabolic health, which can influence hormone balance, ovulation, and pregnancy outcomes. Vively’s continuous glucose monitoring (CGM) program can support you by:

By pairing your AMH insights with Vively’s metabolic tracking, you gain a clearer understanding of how your daily habits impact your fertility and can take proactive steps toward a healthy pregnancy.
AMH testing gives insight into the number of growing follicles in your ovaries, offering a snapshot of your functional ovarian reserve. Studies indicate that AMH is a more reliable indicator of ovarian reserve compared to factors like age, BMI, or FSH levels alone.
This test is particularly useful for fertility planning. It helps guide decisions about treatments such as IVF, egg freezing, and medication dosages. Comparing your AMH levels with others in your age group can also provide additional context about your reproductive health.
That said, AMH is just one factor in the broader picture of fertility.
While AMH is a helpful tool, fertility outcomes are influenced by a wide range of factors, including metabolic health, age, lifestyle, and even your partner's health. This comprehensive approach is especially important considering that infertility affects about 1 in 6 people globally.
Maintaining steady glucose levels, often tracked with a CGM, can support hormonal balance, which is vital for fertility. Conditions like polycystic ovary syndrome (PCOS), which AMH testing can help identify, are frequently tied to metabolic challenges.
If your AMH levels are on the lower side, early action can be crucial. Fertility specialists may recommend trying to conceive sooner or exploring options like egg freezing. Combining your AMH results with a full understanding of your overall health can greatly enhance your chances of reaching your pregnancy goals.
AMH testing plays an important role in evaluating ovarian reserve, giving insight into how many eggs are left in the ovaries. This can be a key piece of the puzzle when it comes to understanding fertility and planning for pregnancy.
To get a fuller picture of fertility health, AMH testing is often combined with other evaluations, such as:
By combining these assessments, you and your healthcare provider can gain a deeper understanding of your fertility and make more informed choices about your family planning goals.
When it comes to Anti-Müllerian Hormone (AMH) levels, age and genetics are the primary factors at play. However, adopting healthier habits can still make a difference in your overall fertility. Eating a nutrient-rich diet filled with antioxidants, vitamins, and healthy fats, paired with consistent moderate exercise, may help support ovarian health and boost reproductive well-being.
In contrast, certain lifestyle choices like smoking, heavy drinking, or dealing with prolonged stress can take a toll on fertility. While these changes might not significantly shift AMH levels, they can contribute to better reproductive health and improve your chances of conceiving.
High Anti-Müllerian Hormone (AMH) levels are frequently associated with polycystic ovary syndrome (PCOS), a condition that disrupts hormone levels and affects ovulation. Elevated AMH usually indicates a higher number of ovarian follicles, which is a hallmark of PCOS.
While having more follicles might sound like a positive sign for fertility, it can actually interfere with ovulation. In cases of PCOS, these follicles often fail to release mature eggs, which can make natural conception more challenging. If you’re dealing with irregular menstrual cycles or struggling to conceive, it’s worth consulting a healthcare provider to explore whether high AMH levels or PCOS could be playing a role.
How does AMH testing contribute to understanding fertility, and what other evaluations should I consider?
AMH testing plays an important role in evaluating ovarian reserve, giving insight into how many eggs are left in the ovaries. This can be a key piece of the puzzle when it comes to understanding fertility and planning for pregnancy.
To get a fuller picture of fertility health, AMH testing is often combined with other evaluations, such as:
By combining these assessments, you and your healthcare provider can gain a deeper understanding of your fertility and make more informed choices about your family planning goals.
When it comes to Anti-Müllerian Hormone (AMH) levels, age and genetics are the primary factors at play. However, adopting healthier habits can still make a difference in your overall fertility. Eating a nutrient-rich diet filled with antioxidants, vitamins, and healthy fats, paired with consistent moderate exercise, may help support ovarian health and boost reproductive well-being.
In contrast, certain lifestyle choices like smoking, heavy drinking, or dealing with prolonged stress can take a toll on fertility. While these changes might not significantly shift AMH levels, they can contribute to better reproductive health and improve your chances of conceiving.
High Anti-Müllerian Hormone (AMH) levels are frequently associated with polycystic ovary syndrome (PCOS), a condition that disrupts hormone levels and affects ovulation. Elevated AMH usually indicates a higher number of ovarian follicles, which is a hallmark of PCOS.
While having more follicles might sound like a positive sign for fertility, it can actually interfere with ovulation. In cases of PCOS, these follicles often fail to release mature eggs, which can make natural conception more challenging. If you’re dealing with irregular menstrual cycles or struggling to conceive, it’s worth consulting a healthcare provider to explore whether high AMH levels or PCOS could be playing a role.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
