Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan




Feeling exhausted no matter how much you sleep? Iron deficiency could be the cause. It affects over two billion people worldwide, especially women of reproductive age. Iron plays a vital role in energy production, oxygen transport, and overall metabolic health.
Key takeaways:
Addressing iron deficiency early can improve energy, blood sugar stability, and overall health. If symptoms persist, consult a doctor for proper testing and guidance.
Iron deficiency often creeps in quietly, with symptoms that are easy to overlook. Early on, the signs may be so mild that they go unnoticed, but as the deficiency worsens, the symptoms become harder to ignore.
This gradual onset means many people delay seeking help, attributing their symptoms to other causes.
One of the most noticeable signs of iron deficiency is persistent fatigue, even after getting plenty of rest. This isn’t the kind of tiredness you feel after a long day—it’s a deep, lingering exhaustion that doesn’t go away with sleep.
Other physical signs to keep an eye on include:
These symptoms can often overlap with other conditions, making it harder to pinpoint iron deficiency as the culprit.
Iron deficiency has a way of mimicking other health issues, which can make diagnosis tricky. Symptoms like fatigue, shortness of breath, and pale skin are common in various conditions, leading to potential misdiagnoses.
Disorders with similar symptoms include allergic rhinitis, anxiety, depression, diabetes, fibromyalgia, influenza, Lyme disease, and thyroid problems.
This overlap is one reason anaemia, particularly iron-deficiency anaemia, is so widespread. Globally, iron deficiency accounts for half of all anaemia cases, with many going undiagnosed for long periods.
Women, in particular, are disproportionately affected. In the United States, only 1% of men under 50 experience iron-deficiency anaemia, but the number jumps to 10% for women of childbearing age. Many women chalk up their fatigue to busy schedules or stress, ignoring the possibility of an underlying deficiency.
If you’ve been feeling unusually tired or noticing other symptoms for more than two weeks, it’s time to consult a healthcare provider. Self-diagnosing or taking iron supplements without proper medical guidance is risky and can lead to complications.
Up next, we’ll dive into how iron deficiency ties into blood sugar regulation and metabolic health.
Wondering how other nutrient deficiencies can impact your energy and wellbeing? Read our guide on vitamin D deficiency in Australia to explore common signs, health risks, and when to get tested.
Iron deficiency can throw off your blood sugar regulation and disrupt your metabolism. This helps explain why many people with low iron levels often feel fatigued, experience energy crashes, and struggle with maintaining metabolic balance.
Iron plays a key role in your body's energy production. When iron levels are low, your cells struggle to produce energy efficiently, which can interfere with how your body processes glucose and responds to insulin.
Studies have shown that low iron levels can affect glucose and fat metabolism while also disrupting insulin signalling pathways. Additionally, iron deficiency is linked to increased glycation of haemoglobin A1C (HbA1c), which might lead to falsely elevated HbA1c readings—a common marker used to assess blood sugar control.
Correcting iron deficiency has been shown to significantly reduce fasting insulin levels and HbA1c values—from 7.4% to 6.2% in some cases. Beyond this, low iron levels can impair insulin's ability to regulate glucose production in the liver. This means the liver may continue producing glucose unnecessarily, leading to higher blood sugar levels.
The fatigue that comes with iron deficiency is more than just feeling tired—it’s a sign that your metabolism is under stress. Low iron affects mitochondrial function, reducing the efficiency of the respiratory chain that powers your muscles.
This diminished energy production can make physical activity harder, which in turn may worsen insulin sensitivity and blood sugar control. On top of that, iron deficiency can increase oxidative stress and insulin resistance.
Certain groups are particularly affected by the link between iron deficiency and metabolic challenges. For instance, iron deficiency anaemia is more common in individuals with type 2 diabetes, especially those dealing with diabetic nephropathy.
A 2014 study even found a direct relationship between iron deficiency and elevated HbA1c levels in a group of 120 people with diabetes and iron deficiency anaemia.
Women often experience a more pronounced impact. Research has shown that iron deficiency is associated with higher odds of having an HbA1c of 5.5% or above (odds ratio 1.39; 95% CI 1.11–1.73).
In non-diabetic premenopausal women with iron deficiency anaemia, addressing the deficiency led to significant reductions in fasting insulin levels and HOMA scores, especially in women under 40 with a normal BMI.
The good news? Restoring iron levels can bring about noticeable metabolic improvements fairly quickly. Early diagnosis and treatment of iron deficiency can lead to better blood sugar control and may even help delay complications. By stabilising glucose levels and improving energy, addressing iron deficiency is essential for maintaining overall metabolic health.
Curious about how your lifestyle affects your ageing process? Learn more in our guide on what your BioAge really means and how to improve it.
Getting tested for iron deficiency involves a mix of traditional lab tests and modern monitoring tools. Together, these methods provide a clearer picture of your iron levels and how they affect your overall health.
When it comes to diagnosing iron deficiency anaemia, serum ferritin is the gold standard. The American Academy of Family Physicians states, "measurement of the serum ferritin level is the most accurate test to diagnose iron deficiency anaemia."
If you're visiting your doctor, ask for this test alongside a complete blood count (CBC), which measures haemoglobin levels and red blood cell size.
Ferritin levels are key for accurate diagnosis. For example, a ferritin level below 30 ng/mL can detect iron deficiency anaemia with 92% sensitivity and 98% specificity. In cases of chronic inflammation, iron deficiency anaemia is more likely when ferritin is under 50 ng/mL, while levels above 100 ng/mL usually rule it out.
If ferritin results leave questions, additional tests like serum iron, transferrin saturation, and total iron-binding capacity (TIBC) may be helpful. TIBC is particularly useful because it increases in severe iron deficiency anaemia but decreases in anaemia linked to chronic disease.
For more complex cases, soluble transferrin receptor testing can provide further insight, as its levels rise with iron deficiency and remain unaffected by inflammation. Interestingly, up to 40% of people with iron deficiency anaemia may have normal red blood cell sizes, making ferritin testing even more critical.
While blood tests remain the cornerstone of diagnosis, emerging technologies are offering new ways to monitor health in real time.
Wearable devices are changing the way we track our health. Research from Stanford Medicine has shown that data from smartwatches can predict dehydration, anaemia, and even illnesses like the flu or a cold.
For instance, shifts in heart rate often correlate with changes in red blood cell count and haemoglobin levels.
Continuous glucose monitoring (CGM) devices, while primarily designed to track glucose, also provide real-time insights into your metabolic health. Subtle changes in your energy levels or overall well-being can sometimes be detected through these tools.
Each testing method has its strengths. Traditional blood tests, like serum ferritin and CBC, provide the clinical accuracy needed for diagnosis and treatment. Meanwhile, wearable devices offer ongoing, real-time insights into your health.
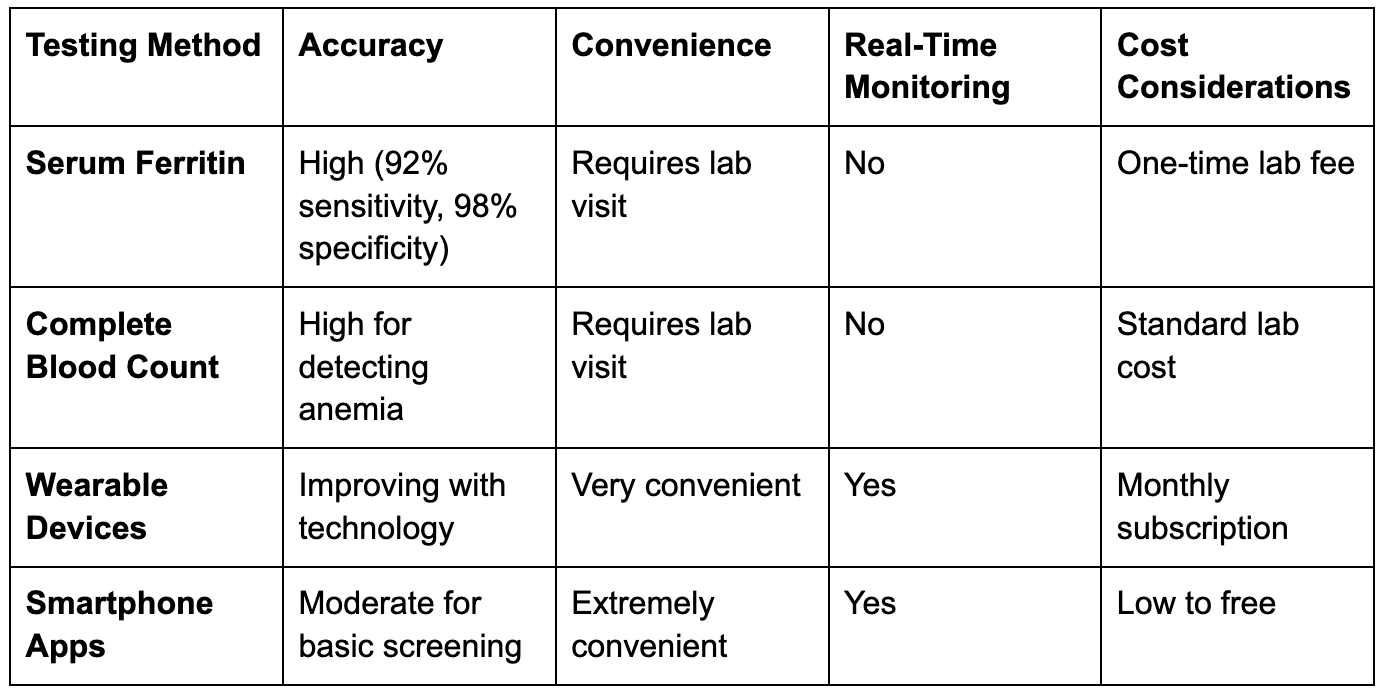
Blood tests remain the most reliable way to diagnose iron deficiency, while wearable devices provide valuable, continuous insights. Considering that anaemia affects roughly 25% of the global population, an integrated approach combining these methods can help avoid misdiagnoses and ensure better health outcomes.
Together, they offer a comprehensive way to assess iron levels and improve metabolic health.
Curious how aerobic fitness factors into your overall health before pregnancy? Learn more about VO₂ max testing and its implications for well‑being.
Tackling iron deficiency involves a mix of smart nutrition, supplements, and tracking tools to restore energy and support a healthy metabolism. When your body is low on iron, it actually absorbs more from your diet—jumping from about 5–10% to as much as 20–30%.
Iron comes in two forms: heme iron (from animal products) and non-heme iron (from plants). Heme iron is absorbed more efficiently, even though it only makes up 10–15% of the average Western diet's iron intake. In fact, it accounts for nearly 40% of the iron your body absorbs.
On the other hand, people eating plant-based diets may only absorb 5–12% of their iron, compared to 14–18% for those consuming animal products.
If you're looking to boost your iron intake, here are some top food options:
For better absorption, pair iron-rich foods with vitamin C sources like oranges, tomatoes, or bell peppers. For example, you could toss orange slices into a spinach salad or drink orange juice with your meal. Timing matters too—coffee and tea can block iron absorption, so avoid them during iron-rich meals. Even cooking with iron cookware can bump up the iron content of your food.
If dietary changes aren’t enough, supplements can help. The most common type is ferrous sulphate, often available in 325 mg tablets. Other options include ferrous gluconate and ferrous fumarate, with ferrous forms generally being easier for your body to absorb.
To get the most out of supplements:
Be cautious about what you consume alongside iron supplements—milk, calcium, antacids, high-fibre foods, and caffeine can block absorption. Common side effects like constipation, nausea, and dark stools are normal. If constipation becomes troublesome, a stool softener might help.
For safety, daily iron intake should stay under 17 mg unless supervised by a doctor. Keep supplements out of children’s reach, as overdoses can be dangerous. If you notice severe symptoms, like tarry stools with red streaks or intense stomach pain, contact your healthcare provider right away.
Iron deficiency doesn’t just affect your energy—it can also disrupt how your body manages glucose. Research shows that people with iron deficiency anaemia often experience greater blood sugar swings and spend more time in hyperglycaemic ranges. Even if you’re not diabetic, low iron levels can impact your glucose stability.
This is where tools like Vively's continuous glucose monitoring (CGM) program come in handy. It provides real-time data on your blood sugar patterns, helping you spot spikes after meals or energy dips tied to glucose levels. As you improve your iron levels through diet or supplements, you might see those blood sugar swings even out—smoother post-meal curves and less variability overall. Vively’s CGM program offers a clear way to track these changes and fine-tune your approach to better metabolic health.
If you're dealing with fatigue and wondering whether iron deficiency or blood sugar swings are to blame, Vively can help you see the bigger picture. While blood tests confirm low iron levels, daily symptoms like exhaustion, poor recovery, or energy dips often point to deeper metabolic imbalances. That’s where continuous data matters.

With Vively, you can:
If you’re working to restore your iron levels and support long-term health, Vively offers real-world data to back up your efforts—so you're not guessing. It’s a practical way to connect how you feel with how your body functions day to day.
Curious about how you can keep tabs on your metabolism from the comfort of home? Discover a step‑by‑step guide on testing your metabolic health easily and accurately.
Iron deficiency impacts about a quarter of the global population and is one of the leading causes of disability worldwide. Addressing it promptly can enhance your quality of life, improve physical health, and reduce fatigue and cognitive challenges.
To tackle iron deficiency, follow these three key steps: identify the deficiency, determine its cause, and replenish your iron levels. Start by watching for symptoms like persistent tiredness, shortness of breath, or unusually pale skin. If these signs appear, confirm the diagnosis through blood tests, such as serum ferritin and transferrin saturation.
Factors like heavy menstrual bleeding, digestive issues, or poor nutrition often contribute to iron deficiency. It's crucial to address the root cause to prevent the problem from recurring.
For replenishing iron levels, oral supplements are a common solution. Ferrous salts, such as gluconate, sulphate, or fumarate, at doses as low as 15–30 mg of elemental iron per day can be effective and better tolerated.
To enhance absorption, take these supplements on an empty stomach with vitamin C, but avoid consuming tea, coffee, or calcium-rich foods at the same time. If oral supplements don't work or cause side effects, intravenous iron may be a better alternative.
Dietary changes are equally important. Incorporate iron-rich foods like dark leafy greens, iron-fortified cereals, beans, nuts, brown rice, meat, fish, and eggs into your meals. Keep in mind that heme iron, found in meat, is absorbed more efficiently than non-heme iron from plant-based foods.
For those with iron deficiency anaemia, higher doses of iron—150–200 mg per day (or 2–5 mg per kilogram)—may be necessary. Once you've adjusted your diet and started supplementation, it’s important to monitor your progress.
Iron levels also tie into blood sugar management. Vively’s continuous glucose monitoring (CGM) program can help you observe how improving your iron stores impacts your blood sugar patterns. As your iron levels recover, you might notice steadier glucose levels and reduced fluctuations throughout the day, making it easier to make smarter dietary and lifestyle choices.
To track your progress, check your haemoglobin levels every 4–8 weeks. With the right combination of diet, iron supplements, and CGM tracking, you can boost your energy levels and support better metabolic health.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Feeling exhausted no matter how much you sleep? Iron deficiency could be the cause. It affects over two billion people worldwide, especially women of reproductive age. Iron plays a vital role in energy production, oxygen transport, and overall metabolic health.
Key takeaways:
Addressing iron deficiency early can improve energy, blood sugar stability, and overall health. If symptoms persist, consult a doctor for proper testing and guidance.
Iron deficiency often creeps in quietly, with symptoms that are easy to overlook. Early on, the signs may be so mild that they go unnoticed, but as the deficiency worsens, the symptoms become harder to ignore.
This gradual onset means many people delay seeking help, attributing their symptoms to other causes.
One of the most noticeable signs of iron deficiency is persistent fatigue, even after getting plenty of rest. This isn’t the kind of tiredness you feel after a long day—it’s a deep, lingering exhaustion that doesn’t go away with sleep.
Other physical signs to keep an eye on include:
These symptoms can often overlap with other conditions, making it harder to pinpoint iron deficiency as the culprit.
Iron deficiency has a way of mimicking other health issues, which can make diagnosis tricky. Symptoms like fatigue, shortness of breath, and pale skin are common in various conditions, leading to potential misdiagnoses.
Disorders with similar symptoms include allergic rhinitis, anxiety, depression, diabetes, fibromyalgia, influenza, Lyme disease, and thyroid problems.
This overlap is one reason anaemia, particularly iron-deficiency anaemia, is so widespread. Globally, iron deficiency accounts for half of all anaemia cases, with many going undiagnosed for long periods.
Women, in particular, are disproportionately affected. In the United States, only 1% of men under 50 experience iron-deficiency anaemia, but the number jumps to 10% for women of childbearing age. Many women chalk up their fatigue to busy schedules or stress, ignoring the possibility of an underlying deficiency.
If you’ve been feeling unusually tired or noticing other symptoms for more than two weeks, it’s time to consult a healthcare provider. Self-diagnosing or taking iron supplements without proper medical guidance is risky and can lead to complications.
Up next, we’ll dive into how iron deficiency ties into blood sugar regulation and metabolic health.
Wondering how other nutrient deficiencies can impact your energy and wellbeing? Read our guide on vitamin D deficiency in Australia to explore common signs, health risks, and when to get tested.
Iron deficiency can throw off your blood sugar regulation and disrupt your metabolism. This helps explain why many people with low iron levels often feel fatigued, experience energy crashes, and struggle with maintaining metabolic balance.
Iron plays a key role in your body's energy production. When iron levels are low, your cells struggle to produce energy efficiently, which can interfere with how your body processes glucose and responds to insulin.
Studies have shown that low iron levels can affect glucose and fat metabolism while also disrupting insulin signalling pathways. Additionally, iron deficiency is linked to increased glycation of haemoglobin A1C (HbA1c), which might lead to falsely elevated HbA1c readings—a common marker used to assess blood sugar control.
Correcting iron deficiency has been shown to significantly reduce fasting insulin levels and HbA1c values—from 7.4% to 6.2% in some cases. Beyond this, low iron levels can impair insulin's ability to regulate glucose production in the liver. This means the liver may continue producing glucose unnecessarily, leading to higher blood sugar levels.
The fatigue that comes with iron deficiency is more than just feeling tired—it’s a sign that your metabolism is under stress. Low iron affects mitochondrial function, reducing the efficiency of the respiratory chain that powers your muscles.
This diminished energy production can make physical activity harder, which in turn may worsen insulin sensitivity and blood sugar control. On top of that, iron deficiency can increase oxidative stress and insulin resistance.
Certain groups are particularly affected by the link between iron deficiency and metabolic challenges. For instance, iron deficiency anaemia is more common in individuals with type 2 diabetes, especially those dealing with diabetic nephropathy.
A 2014 study even found a direct relationship between iron deficiency and elevated HbA1c levels in a group of 120 people with diabetes and iron deficiency anaemia.
Women often experience a more pronounced impact. Research has shown that iron deficiency is associated with higher odds of having an HbA1c of 5.5% or above (odds ratio 1.39; 95% CI 1.11–1.73).
In non-diabetic premenopausal women with iron deficiency anaemia, addressing the deficiency led to significant reductions in fasting insulin levels and HOMA scores, especially in women under 40 with a normal BMI.
The good news? Restoring iron levels can bring about noticeable metabolic improvements fairly quickly. Early diagnosis and treatment of iron deficiency can lead to better blood sugar control and may even help delay complications. By stabilising glucose levels and improving energy, addressing iron deficiency is essential for maintaining overall metabolic health.
Curious about how your lifestyle affects your ageing process? Learn more in our guide on what your BioAge really means and how to improve it.
Getting tested for iron deficiency involves a mix of traditional lab tests and modern monitoring tools. Together, these methods provide a clearer picture of your iron levels and how they affect your overall health.
When it comes to diagnosing iron deficiency anaemia, serum ferritin is the gold standard. The American Academy of Family Physicians states, "measurement of the serum ferritin level is the most accurate test to diagnose iron deficiency anaemia."
If you're visiting your doctor, ask for this test alongside a complete blood count (CBC), which measures haemoglobin levels and red blood cell size.
Ferritin levels are key for accurate diagnosis. For example, a ferritin level below 30 ng/mL can detect iron deficiency anaemia with 92% sensitivity and 98% specificity. In cases of chronic inflammation, iron deficiency anaemia is more likely when ferritin is under 50 ng/mL, while levels above 100 ng/mL usually rule it out.
If ferritin results leave questions, additional tests like serum iron, transferrin saturation, and total iron-binding capacity (TIBC) may be helpful. TIBC is particularly useful because it increases in severe iron deficiency anaemia but decreases in anaemia linked to chronic disease.
For more complex cases, soluble transferrin receptor testing can provide further insight, as its levels rise with iron deficiency and remain unaffected by inflammation. Interestingly, up to 40% of people with iron deficiency anaemia may have normal red blood cell sizes, making ferritin testing even more critical.
While blood tests remain the cornerstone of diagnosis, emerging technologies are offering new ways to monitor health in real time.
Wearable devices are changing the way we track our health. Research from Stanford Medicine has shown that data from smartwatches can predict dehydration, anaemia, and even illnesses like the flu or a cold.
For instance, shifts in heart rate often correlate with changes in red blood cell count and haemoglobin levels.
Continuous glucose monitoring (CGM) devices, while primarily designed to track glucose, also provide real-time insights into your metabolic health. Subtle changes in your energy levels or overall well-being can sometimes be detected through these tools.
Each testing method has its strengths. Traditional blood tests, like serum ferritin and CBC, provide the clinical accuracy needed for diagnosis and treatment. Meanwhile, wearable devices offer ongoing, real-time insights into your health.
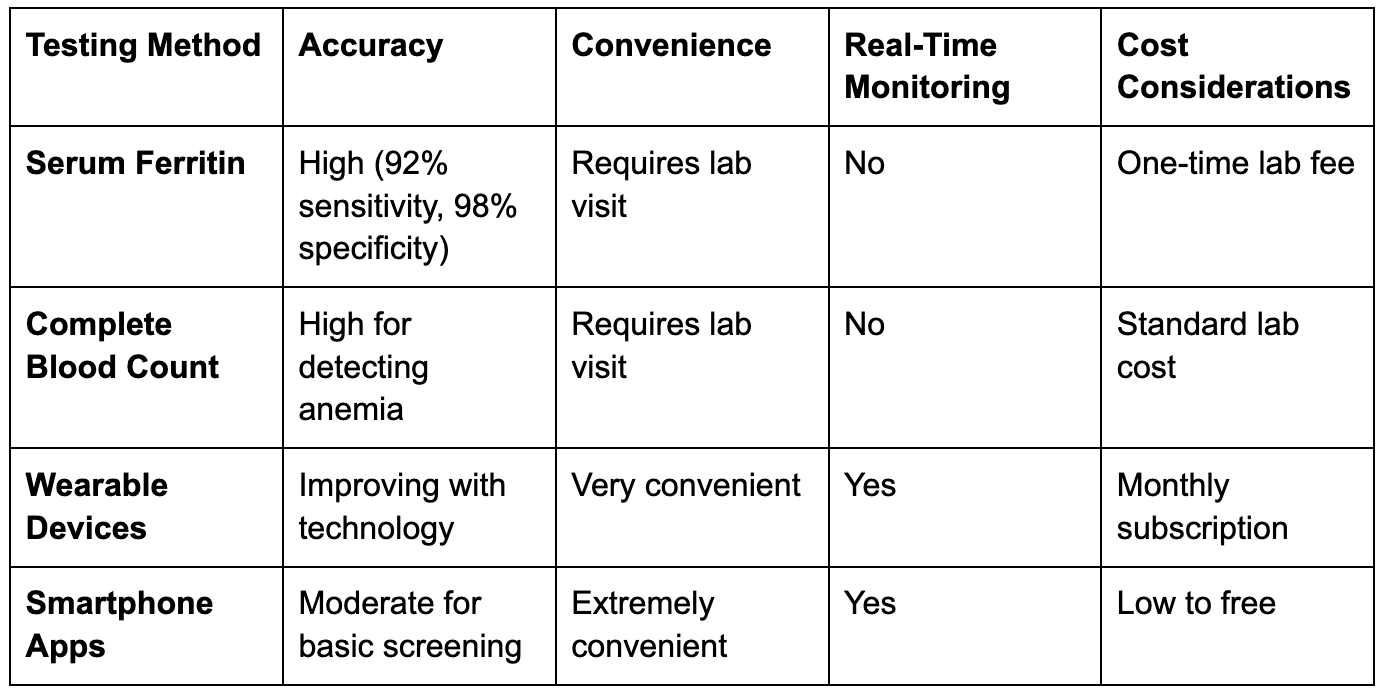
Blood tests remain the most reliable way to diagnose iron deficiency, while wearable devices provide valuable, continuous insights. Considering that anaemia affects roughly 25% of the global population, an integrated approach combining these methods can help avoid misdiagnoses and ensure better health outcomes.
Together, they offer a comprehensive way to assess iron levels and improve metabolic health.
Curious how aerobic fitness factors into your overall health before pregnancy? Learn more about VO₂ max testing and its implications for well‑being.
Tackling iron deficiency involves a mix of smart nutrition, supplements, and tracking tools to restore energy and support a healthy metabolism. When your body is low on iron, it actually absorbs more from your diet—jumping from about 5–10% to as much as 20–30%.
Iron comes in two forms: heme iron (from animal products) and non-heme iron (from plants). Heme iron is absorbed more efficiently, even though it only makes up 10–15% of the average Western diet's iron intake. In fact, it accounts for nearly 40% of the iron your body absorbs.
On the other hand, people eating plant-based diets may only absorb 5–12% of their iron, compared to 14–18% for those consuming animal products.
If you're looking to boost your iron intake, here are some top food options:
For better absorption, pair iron-rich foods with vitamin C sources like oranges, tomatoes, or bell peppers. For example, you could toss orange slices into a spinach salad or drink orange juice with your meal. Timing matters too—coffee and tea can block iron absorption, so avoid them during iron-rich meals. Even cooking with iron cookware can bump up the iron content of your food.
If dietary changes aren’t enough, supplements can help. The most common type is ferrous sulphate, often available in 325 mg tablets. Other options include ferrous gluconate and ferrous fumarate, with ferrous forms generally being easier for your body to absorb.
To get the most out of supplements:
Be cautious about what you consume alongside iron supplements—milk, calcium, antacids, high-fibre foods, and caffeine can block absorption. Common side effects like constipation, nausea, and dark stools are normal. If constipation becomes troublesome, a stool softener might help.
For safety, daily iron intake should stay under 17 mg unless supervised by a doctor. Keep supplements out of children’s reach, as overdoses can be dangerous. If you notice severe symptoms, like tarry stools with red streaks or intense stomach pain, contact your healthcare provider right away.
Iron deficiency doesn’t just affect your energy—it can also disrupt how your body manages glucose. Research shows that people with iron deficiency anaemia often experience greater blood sugar swings and spend more time in hyperglycaemic ranges. Even if you’re not diabetic, low iron levels can impact your glucose stability.
This is where tools like Vively's continuous glucose monitoring (CGM) program come in handy. It provides real-time data on your blood sugar patterns, helping you spot spikes after meals or energy dips tied to glucose levels. As you improve your iron levels through diet or supplements, you might see those blood sugar swings even out—smoother post-meal curves and less variability overall. Vively’s CGM program offers a clear way to track these changes and fine-tune your approach to better metabolic health.
If you're dealing with fatigue and wondering whether iron deficiency or blood sugar swings are to blame, Vively can help you see the bigger picture. While blood tests confirm low iron levels, daily symptoms like exhaustion, poor recovery, or energy dips often point to deeper metabolic imbalances. That’s where continuous data matters.

With Vively, you can:
If you’re working to restore your iron levels and support long-term health, Vively offers real-world data to back up your efforts—so you're not guessing. It’s a practical way to connect how you feel with how your body functions day to day.
Curious about how you can keep tabs on your metabolism from the comfort of home? Discover a step‑by‑step guide on testing your metabolic health easily and accurately.
Iron deficiency impacts about a quarter of the global population and is one of the leading causes of disability worldwide. Addressing it promptly can enhance your quality of life, improve physical health, and reduce fatigue and cognitive challenges.
To tackle iron deficiency, follow these three key steps: identify the deficiency, determine its cause, and replenish your iron levels. Start by watching for symptoms like persistent tiredness, shortness of breath, or unusually pale skin. If these signs appear, confirm the diagnosis through blood tests, such as serum ferritin and transferrin saturation.
Factors like heavy menstrual bleeding, digestive issues, or poor nutrition often contribute to iron deficiency. It's crucial to address the root cause to prevent the problem from recurring.
For replenishing iron levels, oral supplements are a common solution. Ferrous salts, such as gluconate, sulphate, or fumarate, at doses as low as 15–30 mg of elemental iron per day can be effective and better tolerated.
To enhance absorption, take these supplements on an empty stomach with vitamin C, but avoid consuming tea, coffee, or calcium-rich foods at the same time. If oral supplements don't work or cause side effects, intravenous iron may be a better alternative.
Dietary changes are equally important. Incorporate iron-rich foods like dark leafy greens, iron-fortified cereals, beans, nuts, brown rice, meat, fish, and eggs into your meals. Keep in mind that heme iron, found in meat, is absorbed more efficiently than non-heme iron from plant-based foods.
For those with iron deficiency anaemia, higher doses of iron—150–200 mg per day (or 2–5 mg per kilogram)—may be necessary. Once you've adjusted your diet and started supplementation, it’s important to monitor your progress.
Iron levels also tie into blood sugar management. Vively’s continuous glucose monitoring (CGM) program can help you observe how improving your iron stores impacts your blood sugar patterns. As your iron levels recover, you might notice steadier glucose levels and reduced fluctuations throughout the day, making it easier to make smarter dietary and lifestyle choices.
To track your progress, check your haemoglobin levels every 4–8 weeks. With the right combination of diet, iron supplements, and CGM tracking, you can boost your energy levels and support better metabolic health.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
