Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan




Your thyroid plays a vital role in regulating your metabolism, energy levels, and overall health. When thyroid hormones (TSH, T3, and T4) are imbalanced, they can lead to symptoms like fatigue, weight changes, and heart issues.
Regular thyroid testing helps detect these imbalances early, allowing for effective treatment. Here's a quick breakdown:
Thyroid imbalances also impact weight, blood sugar, and metabolic health. Tools like continuous glucose monitors (CGMs) can provide real-time data to manage these effects better. Proper nutrition, regular testing, and wearable devices can help you maintain thyroid and metabolic health effectively.
Thyroid health revolves around three key hormones: TSH, T3, and T4. These hormones operate in a feedback loop similar to a thermostat. The hypothalamus releases TRH, which prompts the pituitary gland to produce TSH.
TSH then stimulates the thyroid gland to produce T4 and T3. When T3 and T4 levels rise, TSH production decreases, and when they drop, TSH levels increase. This process is highly sensitive, as even small changes in T3 and T4 can cause significant shifts in TSH levels due to their log-linear relationship. Let’s explore the specific roles of each hormone.
TSH is central to thyroid regulation. This hormone, produced by the pituitary gland, binds to receptors on thyroid cells, triggering processes that enhance iodide uptake, thyroglobulin production, and thyroperoxidase activity. It also promotes thyroid tissue growth, which can sometimes lead to an enlarged thyroid when the body demands more hormone production.
Doctors often rely on TSH levels as the first step in diagnosing thyroid issues.
T4, or thyroxine, makes up about 80% of the thyroid hormones released into the bloodstream and serves as an inactive precursor to T3. This conversion from T4 to T3 occurs in organs like the liver, kidneys, and muscles. With a half-life of approximately eight days, T4 provides a steady supply for T3 production.
T4 can also convert into reverse T3, a form that may slow metabolism and contribute to fatigue. Factors such as chronic stress and inflammation can influence this process, potentially affecting overall energy levels.
T3, or triiodothyronine, is the active form of thyroid hormone, even though it accounts for only about 20% of thyroid hormone secretion. It directly impacts metabolism, influencing how the body burns calories, regulates heart rate, and controls body temperature and other organ functions.
Most T3 is produced by converting T4 in peripheral tissues through a process called deiodination, ensuring that tissues receive the active hormone they need.
Together, TSH, T4, and T3 provide a comprehensive picture of thyroid health, which is why thyroid testing often measures all three. Each hormone plays a unique role, offering valuable insights into how the thyroid is functioning.
Interested in how lifestyle choices impact chronic illness? Explore our guides on whether chronic disease is in your DNA and how you can take control.
Interpreting thyroid test results involves analysing levels of TSH, T4, and T3 to understand how well your thyroid is functioning.
Different combinations of these hormone levels can point to specific thyroid conditions, each with its own symptoms and potential health issues. Let’s break down the common patterns and what they might mean for your health.
When TSH levels are high and T4 levels are low, it often signals primary hypothyroidism. In this scenario, the pituitary gland produces more TSH to compensate for a thyroid that isn’t functioning properly. This hormonal imbalance disrupts the usual feedback loop between the pituitary and the thyroid.
This condition affects about 5 out of every 100 people in the United States, with women being far more affected than men. In fact, women are 10 times more likely than men to develop Hashimoto's disease, the leading cause of hypothyroidism in areas where iodised salt is widely available.
Symptoms of hypothyroidism tend to develop gradually and may include feeling unusually cold, constipation, unexplained weight gain, sluggish thinking, and low energy levels. These symptoms are often mistaken for aging or stress, but when untreated, they can have a serious impact on quality of life.
If left untreated, hypothyroidism can lead to severe complications, such as heart issues and osteoporosis. Treatment typically involves daily thyroid hormone replacement, usually in the form of levothyroxine, along with regular blood tests to monitor hormone levels and adjust dosages as needed.
Ready to uncover hidden inflammation and protect your metabolic health? Check out our article on how the CRP blood test reveals chronic inflammation.
Low TSH levels paired with high T4 or T3 levels point to hyperthyroidism. In this case, the pituitary gland reduces TSH production in an effort to slow the thyroid down, but the thyroid continues to produce excessive hormones.
The symptoms of hyperthyroidism are often the opposite of hypothyroidism. You might notice a rapid or irregular heartbeat, unexplained weight loss despite an increased appetite, anxiety, trouble sleeping, and sensitivity to heat. Other symptoms can include nervousness, irritability, hyperactivity, fatigue, muscle weakness, diarrhoea, frequent urination, excessive thirst, and reduced interest in sex.
Physical signs to watch for include a goitre (swollen neck), trembling hands, warm and sweaty skin, red palms, brittle nails, itchy rashes, patchy hair loss, and eye issues like dryness, redness, or vision changes. Some people may also experience hot flashes, excessive sweating, irregular menstrual cycles, or even an increased risk of miscarriage.
If you’re experiencing these symptoms, it’s essential to consult a doctor for proper testing. Writing down all your symptoms in advance can help your healthcare provider make a more accurate diagnosis.
Low levels of both TSH and T4 suggest a problem with the pituitary gland, known as secondary hypothyroidism. This happens when the pituitary fails to produce enough TSH to stimulate the thyroid properly.
Secondary hypothyroidism is rare, accounting for fewer than 1% of thyroid-related cases. It often requires further evaluation, such as an MRI and additional hormone tests. The condition can result from various causes, including tumours, inflammation, autoimmune diseases, trauma, or radiation exposure. Its prevalence at birth is estimated to range from 1 in 16,000 to 1 in 100,000 people.
Diagnosing secondary hypothyroidism requires a different approach than primary thyroid disorders.
Additional hormone systems should also be evaluated, such as cortisol, growth hormone, and sex hormones, since pituitary dysfunction often impacts multiple pathways.
Here’s a quick summary of the common patterns:
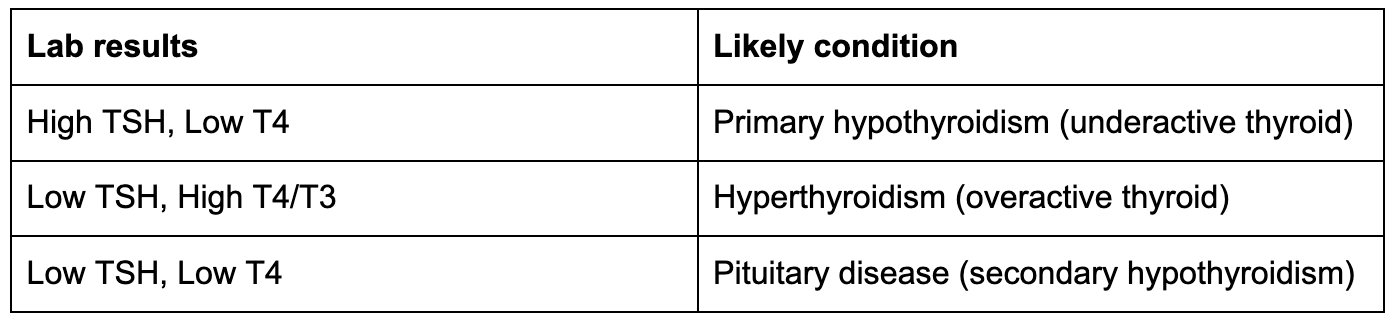
Understanding these hormonal patterns can help you and your healthcare provider identify the underlying cause of your symptoms and create an effective treatment plan.
Your thyroid plays a crucial role in regulating your metabolism. When thyroid hormones are out of balance, the effects can cascade throughout your metabolic system, influencing everything from weight changes to glucose control.
This connection helps explain how thyroid health ties into broader metabolic shifts and highlights the importance of using modern tools for monitoring.
When thyroid hormone levels are high, your basal metabolic rate (BMR) increases, leading to more calorie burn. On the flip side, low thyroid hormone levels slow down your BMR, which can result in weight gain.
Hyperthyroidism, or an overactive thyroid, speeds up metabolism and often causes rapid weight loss even when appetite increases. Hypothyroidism, on the other hand, slows metabolism, leading to weight gain, though this is usually due to water and salt retention rather than fat accumulation.
Once hypothyroidism is treated and hormone levels stabilise, weight regulation becomes similar to that of individuals without thyroid issues.
Thyroid hormones don't just affect weight; they also influence blood sugar regulation. They impact pancreatic β-cell development and glucose metabolism in various organs. A large clinical study involving 1,310 adults with diabetes found thyroid diseases in 13.4% of participants, with higher rates in type 1 diabetes (31.4%) compared to type 2 diabetes (6.9%).
Both hyperthyroidism and hypothyroidism can lead to insulin resistance, but they do so in different ways. Hyperthyroidism increases glucose absorption, liver glucose production, and the release of free fatty acids, overwhelming insulin and reducing its effectiveness.
On the other hand, hypothyroidism slows glucose absorption, delays glucose metabolism, and lowers insulin sensitivity in muscle and fat tissue. These effects contribute to a higher risk of diabetes: people with hyperthyroidism are 43% more likely to develop diabetes, while those with hypothyroidism face a 40% increased prevalence compared to those with normal thyroid function.
These complex changes highlight the value of continuous monitoring to understand and manage these shifts.
Continuous glucose monitors (CGMs) offer real-time insights into how factors like diet, exercise, stress, and sleep impact blood sugar levels. For individuals with thyroid imbalances, CGMs can uncover patterns in glucose metabolism that routine blood tests might miss.
Vively's CGM program transforms glucose data into actionable insights through a combination of a sensor, app, and optional dietitian support. Over 15,000 members have used Vively to identify their unique blood sugar patterns, with 82% reporting better energy levels and 85% noticing improvements in their weight.
For those navigating thyroid-related metabolic challenges, Vively provides a tailored approach. It enables users to track how food choices impact glucose levels during metabolic fluctuations caused by thyroid imbalances. The app also lets you experiment with meal timing, exercise routines, and sleep schedules to find what works best for your body.
Plus, the optional dietitian support offers personalised guidance from registered professionals, making it easier to manage these complex changes effectively.
“Thyroid health is deeply connected to your metabolism. Understanding your TSH, T3, and T4 levels gives you the power to make targeted changes that support both energy and long-term wellbeing. With Vively’s continuous glucose monitoring, you can see how these hormonal shifts influence your blood sugar and make real-time adjustments to improve your health.” — Dr Michelle Woolhouse, Integrative GP & Founding Medical Director at Vively
Understanding thyroid tests and combining them with real-time glucose data can help you make more precise decisions about your metabolic health. With regular testing, tailored nutrition, and modern wearable technology, you can actively manage and improve thyroid and metabolic function. Below, you'll find practical ways to incorporate these tools into your daily routine.
How often you should test your thyroid depends on your health and specific circumstances. The American Thyroid Association suggests thyroid function tests for all adults starting at age 35, with follow-ups every five years. If you're managing hypothyroidism, more frequent testing is necessary. For primary hypothyroidism, TSH and free T4 levels should be checked every six weeks during medication adjustments and annually once stabilised.
Secondary hypothyroidism monitoring focuses on free T4, following a similar schedule.
Women over 50, those with thyroid-related symptoms, or individuals with a family history of thyroid issues should have more frequent screenings. If you're on medications that impact thyroid function, a full thyroid panel is recommended before starting the treatment, followed by tests within six months and then every 6 to 12 months.
Pregnancy adds another layer of importance to thyroid monitoring. During the first trimester, TSH levels should range between 0.1 and 2.5 mIU/L, with follow-ups every four weeks until 20 weeks and an additional test at 30 weeks. Testing six weeks postpartum is also advised.
Eating the right nutrients is crucial for thyroid function. A diet rich in iodine, selenium, zinc, vitamin D, vitamin B12, magnesium, and iron can support thyroid health. For iodine, include seaweed, fish, dairy, and iodised salt.
Selenium can be found in Brazil nuts, eggs, and tuna, while lean meats, spinach, pumpkin seeds, and whole grains provide iron and zinc. Be cautious with excess iodine, as it can disrupt thyroid function.
Vitamin D deficiency has been linked to autoimmune thyroid conditions, so aim for sunlight exposure or consider supplements. Vitamin B12, found in milk, eggs, fish, and meat, also plays a role in maintaining thyroid health.
Limiting processed foods, refined sugars, and artificial additives is equally important. Additionally, moderate your intake of soy products and cruciferous vegetables, as these can interfere with thyroid function when consumed in large quantities. Focus on whole, nutrient-rich foods to support both thyroid and overall metabolic health.
Thyroid health and metabolism are closely connected, and wearable technology can provide deeper insights. Combining traditional thyroid tests with real-time data from devices like continuous glucose monitors (CGMs) offer a more dynamic understanding of how your thyroid function impacts daily metabolic patterns. CGMs can reveal glucose fluctuations that standard tests might overlook.
This is particularly helpful for those with thyroid imbalances, as it shows how thyroid function influences blood sugar levels throughout the day in response to meals and activities.
Wearables also track sleep quality, heart rate, stress, and physical activity. Paired with thyroid test results, this data creates a fuller picture of your metabolic health. For instance, you might notice that poor sleep coincides with glucose level changes during periods of low thyroid function.
AI-powered analysis of CGM data can even detect subtle patterns that signal a higher risk for type 2 diabetes. In one pilot study in rural India, AI-driven interventions improved glycaemic control by 18% among prediabetic participants.
By integrating thyroid testing with wearable data, you can receive personalised feedback and actionable recommendations. This combination turns static lab results into meaningful insights, helping you fine-tune meal timing, physical activity, and other lifestyle factors for better metabolic health.
Need a comprehensive check-up for your overall wellbeing? Explore our guide on how to get a full body check in Australia and what tests to consider.
Understanding your TSH, T3, and T4 levels gives you the tools to actively manage your metabolic health.
With 20 million Americans dealing with thyroid disorders and thyroid dysfunction affecting 31.9% of metabolic syndrome patients, knowing your test results can help spot potential issues before they escalate into serious health concerns. This knowledge lays the groundwork for using advanced testing and monitoring tools to stay ahead.
While TSH screening is a common starting point, a full thyroid panel offers a more detailed picture. This includes free T3, free T4, reverse T3, and thyroid antibodies. Although TSH testing identifies most thyroid problems, relying solely on it can miss up to 7% of imbalances.
Modern wearables add another layer of insight by offering real-time metabolic data that traditional lab tests can't provide.
For instance, research has shown that an increase in resting heart rate by about 11 beats per minute, detected through a wearable device, correlates with a 0.5 ng/dL rise in serum free thyroxine levels and a 3.8 times greater risk of thyrotoxicosis. By combining lab results with wearable data, you can quickly adapt your diet, exercise, and treatment strategies.
Thyroid hormones play a critical role in metabolism, and integrating traditional testing with modern monitoring can deliver substantial benefits. For example, studies show that using advanced continuous glucose monitoring (CGM) technologies led to a 15-20% decrease in hypoglycemic events and better HbA1c levels over six months. Additionally, effectively managing endocrine disorders can lower the risk of cardiovascular events by up to 25%.
Being proactive is key to taking control. Pay attention to symptoms like unexplained fatigue, weight changes, mood shifts, or sensitivity to temperature. Regular hormone testing allows for timely interventions, while wearable devices help you track how thyroid function influences your daily activities, sleep quality, and glucose levels.
Combining expert medical advice with data from wearables creates a powerful approach to managing your metabolic health. Your thyroid plays a central role in regulating energy, maintaining stable blood sugar, and supporting heart health. With a mix of regular testing, symptom awareness, and modern monitoring tools, you can make informed decisions to improve your metabolic health for the long haul.
TSH, T3, and T4 hormones are essential for keeping your metabolism on track, directly influencing how your body uses energy and manages weight. T3, often called the active thyroid hormone, plays a key role in determining how efficiently your cells burn calories. When T3 levels are higher, your metabolism tends to speed up, leading to increased energy use and possible weight loss. On the flip side, lower T3 levels can slow things down, making weight gain more likely.
TSH (thyroid-stimulating hormone) acts as the regulator, controlling the production of T3 and T4. Elevated TSH levels often point to an underactive thyroid, or hypothyroidism, which can slow your metabolism, leaving you feeling tired and prone to weight gain. On the other hand, low TSH levels might indicate an overactive thyroid, or hyperthyroidism, which can ramp up your metabolism and result in weight loss. Keeping tabs on these hormone levels is crucial for effectively managing thyroid-related metabolic challenges.
If hypothyroidism isn't treated, it can cause serious health problems like heart disease, nerve damage, a swollen thyroid gland (goiter), major weight gain, and memory or concentration issues, often referred to as "brain fog."
Similarly, untreated hyperthyroidism can lead to severe heart problems, weakened bones (osteoporosis), and fertility challenges. Both conditions can deeply affect your quality of life, making early diagnosis and treatment essential to avoid lasting health complications.
Continuous glucose monitors (CGMs) provide real-time data on blood sugar levels, allowing you to spot patterns and fluctuations that may be tied to thyroid conditions. Since thyroid issues can interfere with how your body processes glucose, using a CGM can give you a clearer picture of your metabolic health.
With this information, you and your healthcare provider can fine-tune your diet, lifestyle, or treatment plan to address thyroid-related metabolic challenges. This hands-on approach supports better symptom control and promotes overall well-being.
How do TSH, T3, and T4 levels impact metabolism and weight management?
TSH, T3, and T4 hormones are essential for keeping your metabolism on track, directly influencing how your body uses energy and manages weight. T3, often called the active thyroid hormone, plays a key role in determining how efficiently your cells burn calories. When T3 levels are higher, your metabolism tends to speed up, leading to increased energy use and possible weight loss. On the flip side, lower T3 levels can slow things down, making weight gain more likely.
TSH (thyroid-stimulating hormone) acts as the regulator, controlling the production of T3 and T4. Elevated TSH levels often point to an underactive thyroid, or hypothyroidism, which can slow your metabolism, leaving you feeling tired and prone to weight gain. On the other hand, low TSH levels might indicate an overactive thyroid, or hyperthyroidism, which can ramp up your metabolism and result in weight loss. Keeping tabs on these hormone levels is crucial for effectively managing thyroid-related metabolic challenges.
If hypothyroidism isn't treated, it can cause serious health problems like heart disease, nerve damage, a swollen thyroid gland (goiter), major weight gain, and memory or concentration issues, often referred to as "brain fog."
Similarly, untreated hyperthyroidism can lead to severe heart problems, weakened bones (osteoporosis), and fertility challenges. Both conditions can deeply affect your quality of life, making early diagnosis and treatment essential to avoid lasting health complications.
Continuous glucose monitors (CGMs) provide real-time data on blood sugar levels, allowing you to spot patterns and fluctuations that may be tied to thyroid conditions. Since thyroid issues can interfere with how your body processes glucose, using a CGM can give you a clearer picture of your metabolic health.
With this information, you and your healthcare provider can fine-tune your diet, lifestyle, or treatment plan to address thyroid-related metabolic challenges. This hands-on approach supports better symptom control and promotes overall well-being.
Subscribe to our newsletter & join a community of 20,000+ Aussies
.png)
Your thyroid plays a vital role in regulating your metabolism, energy levels, and overall health. When thyroid hormones (TSH, T3, and T4) are imbalanced, they can lead to symptoms like fatigue, weight changes, and heart issues.
Regular thyroid testing helps detect these imbalances early, allowing for effective treatment. Here's a quick breakdown:
Thyroid imbalances also impact weight, blood sugar, and metabolic health. Tools like continuous glucose monitors (CGMs) can provide real-time data to manage these effects better. Proper nutrition, regular testing, and wearable devices can help you maintain thyroid and metabolic health effectively.
Thyroid health revolves around three key hormones: TSH, T3, and T4. These hormones operate in a feedback loop similar to a thermostat. The hypothalamus releases TRH, which prompts the pituitary gland to produce TSH.
TSH then stimulates the thyroid gland to produce T4 and T3. When T3 and T4 levels rise, TSH production decreases, and when they drop, TSH levels increase. This process is highly sensitive, as even small changes in T3 and T4 can cause significant shifts in TSH levels due to their log-linear relationship. Let’s explore the specific roles of each hormone.
TSH is central to thyroid regulation. This hormone, produced by the pituitary gland, binds to receptors on thyroid cells, triggering processes that enhance iodide uptake, thyroglobulin production, and thyroperoxidase activity. It also promotes thyroid tissue growth, which can sometimes lead to an enlarged thyroid when the body demands more hormone production.
Doctors often rely on TSH levels as the first step in diagnosing thyroid issues.
T4, or thyroxine, makes up about 80% of the thyroid hormones released into the bloodstream and serves as an inactive precursor to T3. This conversion from T4 to T3 occurs in organs like the liver, kidneys, and muscles. With a half-life of approximately eight days, T4 provides a steady supply for T3 production.
T4 can also convert into reverse T3, a form that may slow metabolism and contribute to fatigue. Factors such as chronic stress and inflammation can influence this process, potentially affecting overall energy levels.
T3, or triiodothyronine, is the active form of thyroid hormone, even though it accounts for only about 20% of thyroid hormone secretion. It directly impacts metabolism, influencing how the body burns calories, regulates heart rate, and controls body temperature and other organ functions.
Most T3 is produced by converting T4 in peripheral tissues through a process called deiodination, ensuring that tissues receive the active hormone they need.
Together, TSH, T4, and T3 provide a comprehensive picture of thyroid health, which is why thyroid testing often measures all three. Each hormone plays a unique role, offering valuable insights into how the thyroid is functioning.
Interested in how lifestyle choices impact chronic illness? Explore our guides on whether chronic disease is in your DNA and how you can take control.
Interpreting thyroid test results involves analysing levels of TSH, T4, and T3 to understand how well your thyroid is functioning.
Different combinations of these hormone levels can point to specific thyroid conditions, each with its own symptoms and potential health issues. Let’s break down the common patterns and what they might mean for your health.
When TSH levels are high and T4 levels are low, it often signals primary hypothyroidism. In this scenario, the pituitary gland produces more TSH to compensate for a thyroid that isn’t functioning properly. This hormonal imbalance disrupts the usual feedback loop between the pituitary and the thyroid.
This condition affects about 5 out of every 100 people in the United States, with women being far more affected than men. In fact, women are 10 times more likely than men to develop Hashimoto's disease, the leading cause of hypothyroidism in areas where iodised salt is widely available.
Symptoms of hypothyroidism tend to develop gradually and may include feeling unusually cold, constipation, unexplained weight gain, sluggish thinking, and low energy levels. These symptoms are often mistaken for aging or stress, but when untreated, they can have a serious impact on quality of life.
If left untreated, hypothyroidism can lead to severe complications, such as heart issues and osteoporosis. Treatment typically involves daily thyroid hormone replacement, usually in the form of levothyroxine, along with regular blood tests to monitor hormone levels and adjust dosages as needed.
Ready to uncover hidden inflammation and protect your metabolic health? Check out our article on how the CRP blood test reveals chronic inflammation.
Low TSH levels paired with high T4 or T3 levels point to hyperthyroidism. In this case, the pituitary gland reduces TSH production in an effort to slow the thyroid down, but the thyroid continues to produce excessive hormones.
The symptoms of hyperthyroidism are often the opposite of hypothyroidism. You might notice a rapid or irregular heartbeat, unexplained weight loss despite an increased appetite, anxiety, trouble sleeping, and sensitivity to heat. Other symptoms can include nervousness, irritability, hyperactivity, fatigue, muscle weakness, diarrhoea, frequent urination, excessive thirst, and reduced interest in sex.
Physical signs to watch for include a goitre (swollen neck), trembling hands, warm and sweaty skin, red palms, brittle nails, itchy rashes, patchy hair loss, and eye issues like dryness, redness, or vision changes. Some people may also experience hot flashes, excessive sweating, irregular menstrual cycles, or even an increased risk of miscarriage.
If you’re experiencing these symptoms, it’s essential to consult a doctor for proper testing. Writing down all your symptoms in advance can help your healthcare provider make a more accurate diagnosis.
Low levels of both TSH and T4 suggest a problem with the pituitary gland, known as secondary hypothyroidism. This happens when the pituitary fails to produce enough TSH to stimulate the thyroid properly.
Secondary hypothyroidism is rare, accounting for fewer than 1% of thyroid-related cases. It often requires further evaluation, such as an MRI and additional hormone tests. The condition can result from various causes, including tumours, inflammation, autoimmune diseases, trauma, or radiation exposure. Its prevalence at birth is estimated to range from 1 in 16,000 to 1 in 100,000 people.
Diagnosing secondary hypothyroidism requires a different approach than primary thyroid disorders.
Additional hormone systems should also be evaluated, such as cortisol, growth hormone, and sex hormones, since pituitary dysfunction often impacts multiple pathways.
Here’s a quick summary of the common patterns:
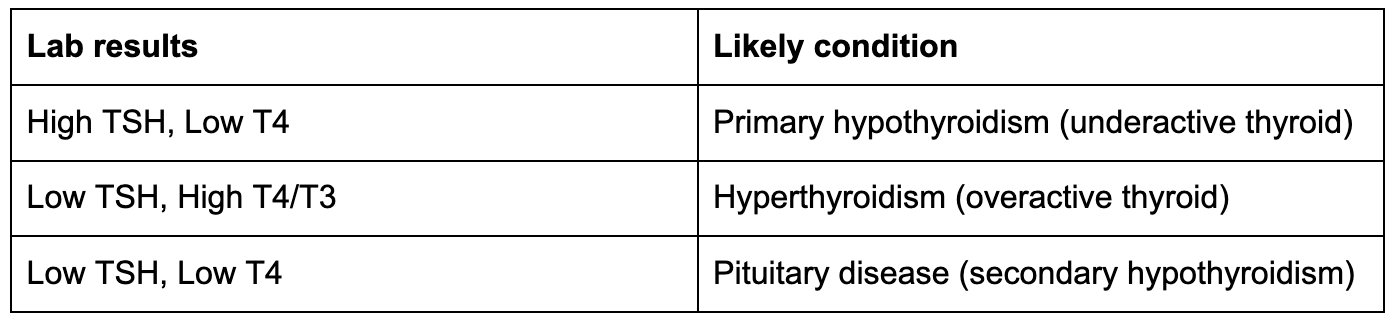
Understanding these hormonal patterns can help you and your healthcare provider identify the underlying cause of your symptoms and create an effective treatment plan.
Your thyroid plays a crucial role in regulating your metabolism. When thyroid hormones are out of balance, the effects can cascade throughout your metabolic system, influencing everything from weight changes to glucose control.
This connection helps explain how thyroid health ties into broader metabolic shifts and highlights the importance of using modern tools for monitoring.
When thyroid hormone levels are high, your basal metabolic rate (BMR) increases, leading to more calorie burn. On the flip side, low thyroid hormone levels slow down your BMR, which can result in weight gain.
Hyperthyroidism, or an overactive thyroid, speeds up metabolism and often causes rapid weight loss even when appetite increases. Hypothyroidism, on the other hand, slows metabolism, leading to weight gain, though this is usually due to water and salt retention rather than fat accumulation.
Once hypothyroidism is treated and hormone levels stabilise, weight regulation becomes similar to that of individuals without thyroid issues.
Thyroid hormones don't just affect weight; they also influence blood sugar regulation. They impact pancreatic β-cell development and glucose metabolism in various organs. A large clinical study involving 1,310 adults with diabetes found thyroid diseases in 13.4% of participants, with higher rates in type 1 diabetes (31.4%) compared to type 2 diabetes (6.9%).
Both hyperthyroidism and hypothyroidism can lead to insulin resistance, but they do so in different ways. Hyperthyroidism increases glucose absorption, liver glucose production, and the release of free fatty acids, overwhelming insulin and reducing its effectiveness.
On the other hand, hypothyroidism slows glucose absorption, delays glucose metabolism, and lowers insulin sensitivity in muscle and fat tissue. These effects contribute to a higher risk of diabetes: people with hyperthyroidism are 43% more likely to develop diabetes, while those with hypothyroidism face a 40% increased prevalence compared to those with normal thyroid function.
These complex changes highlight the value of continuous monitoring to understand and manage these shifts.
Continuous glucose monitors (CGMs) offer real-time insights into how factors like diet, exercise, stress, and sleep impact blood sugar levels. For individuals with thyroid imbalances, CGMs can uncover patterns in glucose metabolism that routine blood tests might miss.
Vively's CGM program transforms glucose data into actionable insights through a combination of a sensor, app, and optional dietitian support. Over 15,000 members have used Vively to identify their unique blood sugar patterns, with 82% reporting better energy levels and 85% noticing improvements in their weight.
For those navigating thyroid-related metabolic challenges, Vively provides a tailored approach. It enables users to track how food choices impact glucose levels during metabolic fluctuations caused by thyroid imbalances. The app also lets you experiment with meal timing, exercise routines, and sleep schedules to find what works best for your body.
Plus, the optional dietitian support offers personalised guidance from registered professionals, making it easier to manage these complex changes effectively.
“Thyroid health is deeply connected to your metabolism. Understanding your TSH, T3, and T4 levels gives you the power to make targeted changes that support both energy and long-term wellbeing. With Vively’s continuous glucose monitoring, you can see how these hormonal shifts influence your blood sugar and make real-time adjustments to improve your health.” — Dr Michelle Woolhouse, Integrative GP & Founding Medical Director at Vively
Understanding thyroid tests and combining them with real-time glucose data can help you make more precise decisions about your metabolic health. With regular testing, tailored nutrition, and modern wearable technology, you can actively manage and improve thyroid and metabolic function. Below, you'll find practical ways to incorporate these tools into your daily routine.
How often you should test your thyroid depends on your health and specific circumstances. The American Thyroid Association suggests thyroid function tests for all adults starting at age 35, with follow-ups every five years. If you're managing hypothyroidism, more frequent testing is necessary. For primary hypothyroidism, TSH and free T4 levels should be checked every six weeks during medication adjustments and annually once stabilised.
Secondary hypothyroidism monitoring focuses on free T4, following a similar schedule.
Women over 50, those with thyroid-related symptoms, or individuals with a family history of thyroid issues should have more frequent screenings. If you're on medications that impact thyroid function, a full thyroid panel is recommended before starting the treatment, followed by tests within six months and then every 6 to 12 months.
Pregnancy adds another layer of importance to thyroid monitoring. During the first trimester, TSH levels should range between 0.1 and 2.5 mIU/L, with follow-ups every four weeks until 20 weeks and an additional test at 30 weeks. Testing six weeks postpartum is also advised.
Eating the right nutrients is crucial for thyroid function. A diet rich in iodine, selenium, zinc, vitamin D, vitamin B12, magnesium, and iron can support thyroid health. For iodine, include seaweed, fish, dairy, and iodised salt.
Selenium can be found in Brazil nuts, eggs, and tuna, while lean meats, spinach, pumpkin seeds, and whole grains provide iron and zinc. Be cautious with excess iodine, as it can disrupt thyroid function.
Vitamin D deficiency has been linked to autoimmune thyroid conditions, so aim for sunlight exposure or consider supplements. Vitamin B12, found in milk, eggs, fish, and meat, also plays a role in maintaining thyroid health.
Limiting processed foods, refined sugars, and artificial additives is equally important. Additionally, moderate your intake of soy products and cruciferous vegetables, as these can interfere with thyroid function when consumed in large quantities. Focus on whole, nutrient-rich foods to support both thyroid and overall metabolic health.
Thyroid health and metabolism are closely connected, and wearable technology can provide deeper insights. Combining traditional thyroid tests with real-time data from devices like continuous glucose monitors (CGMs) offer a more dynamic understanding of how your thyroid function impacts daily metabolic patterns. CGMs can reveal glucose fluctuations that standard tests might overlook.
This is particularly helpful for those with thyroid imbalances, as it shows how thyroid function influences blood sugar levels throughout the day in response to meals and activities.
Wearables also track sleep quality, heart rate, stress, and physical activity. Paired with thyroid test results, this data creates a fuller picture of your metabolic health. For instance, you might notice that poor sleep coincides with glucose level changes during periods of low thyroid function.
AI-powered analysis of CGM data can even detect subtle patterns that signal a higher risk for type 2 diabetes. In one pilot study in rural India, AI-driven interventions improved glycaemic control by 18% among prediabetic participants.
By integrating thyroid testing with wearable data, you can receive personalised feedback and actionable recommendations. This combination turns static lab results into meaningful insights, helping you fine-tune meal timing, physical activity, and other lifestyle factors for better metabolic health.
Need a comprehensive check-up for your overall wellbeing? Explore our guide on how to get a full body check in Australia and what tests to consider.
Understanding your TSH, T3, and T4 levels gives you the tools to actively manage your metabolic health.
With 20 million Americans dealing with thyroid disorders and thyroid dysfunction affecting 31.9% of metabolic syndrome patients, knowing your test results can help spot potential issues before they escalate into serious health concerns. This knowledge lays the groundwork for using advanced testing and monitoring tools to stay ahead.
While TSH screening is a common starting point, a full thyroid panel offers a more detailed picture. This includes free T3, free T4, reverse T3, and thyroid antibodies. Although TSH testing identifies most thyroid problems, relying solely on it can miss up to 7% of imbalances.
Modern wearables add another layer of insight by offering real-time metabolic data that traditional lab tests can't provide.
For instance, research has shown that an increase in resting heart rate by about 11 beats per minute, detected through a wearable device, correlates with a 0.5 ng/dL rise in serum free thyroxine levels and a 3.8 times greater risk of thyrotoxicosis. By combining lab results with wearable data, you can quickly adapt your diet, exercise, and treatment strategies.
Thyroid hormones play a critical role in metabolism, and integrating traditional testing with modern monitoring can deliver substantial benefits. For example, studies show that using advanced continuous glucose monitoring (CGM) technologies led to a 15-20% decrease in hypoglycemic events and better HbA1c levels over six months. Additionally, effectively managing endocrine disorders can lower the risk of cardiovascular events by up to 25%.
Being proactive is key to taking control. Pay attention to symptoms like unexplained fatigue, weight changes, mood shifts, or sensitivity to temperature. Regular hormone testing allows for timely interventions, while wearable devices help you track how thyroid function influences your daily activities, sleep quality, and glucose levels.
Combining expert medical advice with data from wearables creates a powerful approach to managing your metabolic health. Your thyroid plays a central role in regulating energy, maintaining stable blood sugar, and supporting heart health. With a mix of regular testing, symptom awareness, and modern monitoring tools, you can make informed decisions to improve your metabolic health for the long haul.
TSH, T3, and T4 hormones are essential for keeping your metabolism on track, directly influencing how your body uses energy and manages weight. T3, often called the active thyroid hormone, plays a key role in determining how efficiently your cells burn calories. When T3 levels are higher, your metabolism tends to speed up, leading to increased energy use and possible weight loss. On the flip side, lower T3 levels can slow things down, making weight gain more likely.
TSH (thyroid-stimulating hormone) acts as the regulator, controlling the production of T3 and T4. Elevated TSH levels often point to an underactive thyroid, or hypothyroidism, which can slow your metabolism, leaving you feeling tired and prone to weight gain. On the other hand, low TSH levels might indicate an overactive thyroid, or hyperthyroidism, which can ramp up your metabolism and result in weight loss. Keeping tabs on these hormone levels is crucial for effectively managing thyroid-related metabolic challenges.
If hypothyroidism isn't treated, it can cause serious health problems like heart disease, nerve damage, a swollen thyroid gland (goiter), major weight gain, and memory or concentration issues, often referred to as "brain fog."
Similarly, untreated hyperthyroidism can lead to severe heart problems, weakened bones (osteoporosis), and fertility challenges. Both conditions can deeply affect your quality of life, making early diagnosis and treatment essential to avoid lasting health complications.
Continuous glucose monitors (CGMs) provide real-time data on blood sugar levels, allowing you to spot patterns and fluctuations that may be tied to thyroid conditions. Since thyroid issues can interfere with how your body processes glucose, using a CGM can give you a clearer picture of your metabolic health.
With this information, you and your healthcare provider can fine-tune your diet, lifestyle, or treatment plan to address thyroid-related metabolic challenges. This hands-on approach supports better symptom control and promotes overall well-being.
How do TSH, T3, and T4 levels impact metabolism and weight management?
TSH, T3, and T4 hormones are essential for keeping your metabolism on track, directly influencing how your body uses energy and manages weight. T3, often called the active thyroid hormone, plays a key role in determining how efficiently your cells burn calories. When T3 levels are higher, your metabolism tends to speed up, leading to increased energy use and possible weight loss. On the flip side, lower T3 levels can slow things down, making weight gain more likely.
TSH (thyroid-stimulating hormone) acts as the regulator, controlling the production of T3 and T4. Elevated TSH levels often point to an underactive thyroid, or hypothyroidism, which can slow your metabolism, leaving you feeling tired and prone to weight gain. On the other hand, low TSH levels might indicate an overactive thyroid, or hyperthyroidism, which can ramp up your metabolism and result in weight loss. Keeping tabs on these hormone levels is crucial for effectively managing thyroid-related metabolic challenges.
If hypothyroidism isn't treated, it can cause serious health problems like heart disease, nerve damage, a swollen thyroid gland (goiter), major weight gain, and memory or concentration issues, often referred to as "brain fog."
Similarly, untreated hyperthyroidism can lead to severe heart problems, weakened bones (osteoporosis), and fertility challenges. Both conditions can deeply affect your quality of life, making early diagnosis and treatment essential to avoid lasting health complications.
Continuous glucose monitors (CGMs) provide real-time data on blood sugar levels, allowing you to spot patterns and fluctuations that may be tied to thyroid conditions. Since thyroid issues can interfere with how your body processes glucose, using a CGM can give you a clearer picture of your metabolic health.
With this information, you and your healthcare provider can fine-tune your diet, lifestyle, or treatment plan to address thyroid-related metabolic challenges. This hands-on approach supports better symptom control and promotes overall well-being.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
