Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan




LDL cholesterol alone isn’t enough to assess your heart health. Many people with normal LDL levels still face heart attacks, while others with high LDL remain unaffected. That’s where ApoB and Lipoprotein(a) (Lp(a)) come in.
These advanced markers provide a clearer picture of cardiovascular risk by focusing on the number of harmful particles in your blood and genetic factors that standard tests miss.
Talk to your doctor about these tests and take control of your heart health by combining advanced lipid testing with healthy lifestyle choices.
ApoB and Lipoprotein(a) provide insights that go beyond what traditional cholesterol tests can reveal. While standard cholesterol measurements focus on the amount of cholesterol in the blood, these markers shed light on the number of atherogenic particles and highlight genetic factors that influence cardiovascular risk.
Let’s break down how each of these markers plays a role in heart disease and increases risk.
ApoB (apolipoprotein B) is a crucial structural protein found in all atherogenic lipoproteins. It comes in two forms ApoB48 and ApoB100 with ApoB100 being the one most relevant to heart health. Produced in the liver, ApoB100 is present on lipoproteins like VLDL, IDL, and LDL. Each atherogenic particle carries exactly one ApoB molecule, meaning the concentration of ApoB directly reflects the number of harmful particles in the bloodstream. When these particles get trapped in arterial walls, they spark inflammation and plaque buildup, significantly raising the risk of heart attacks.
Interestingly, ApoB and LDL cholesterol levels don’t always align. Research shows that in about 20% of patients, especially those with high triglycerides, type 2 diabetes, or obesity, ApoB levels can be elevated even when LDL cholesterol appears normal. This means someone with "healthy" LDL cholesterol might still face a heightened risk of heart disease if their ApoB levels are high.
Lipoprotein(a), often abbreviated as Lp(a), adds a unique layer of risk due to its strong genetic component. Lp(a) consists of an LDL particle attached to an additional protein called apolipoprotein(a). Genetics determine 70% to 90% of Lp(a) levels, so lifestyle changes have little impact on reducing its concentration.
Unlike LDL, Lp(a) not only contributes to plaque buildup but also promotes blood clotting and inflammation. This combination increases the risk of heart attack, stroke, aortic valve narrowing, and peripheral artery disease. Levels of Lp(a) above 50 mg/dL (125 nmol/L) are linked to a significantly higher risk of cardiovascular events.
Certain groups, such as individuals of African descent or South Asian heritage, tend to have higher average Lp(a) levels. Additionally, a genetic variation called the KIV2 copy number variant explains much of the variability in Lp(a) levels between individuals.
Studies consistently show that ApoB and Lp(a) are better predictors of cardiovascular risk than traditional cholesterol measurements. A systematic review found that ApoB outperformed LDL cholesterol in predicting cardiovascular events across all studies analyzed.
Similarly, a meta-analysis published in The Lancet highlighted that counting atherogenic particles via ApoB offers a clearer picture of risk compared to focusing solely on the cholesterol content in LDL or non-HDL particles.
For Lp(a), data from the UK Biobank cohort revealed that its association with cardiovascular disease risk is over six times stronger than that of LDL particles. Globally, elevated Lp(a) levels affect more than 1.5 billion people and are linked to a 31% higher risk of cardiovascular disease and a 42% greater chance of an atherosclerotic event.
Even when LDL cholesterol is well-controlled, Lp(a) remains an independent risk factor, with cardiovascular risk rising by 11% for every 50 nmol/L increase in Lp(a). At concentrations above 180 mg/dL, Lp(a)-related cardiovascular risk mirrors that seen in patients with heterozygous familial hypercholesterolemia.
These findings highlight why measuring ApoB and Lp(a) during routine cardiovascular evaluations can provide a more complete understanding of heart disease risk.
Want to know which tests can help you live healthier for longer? Read our guide on the top five longevity biomarkers and how they can guide your health decisions.
Understanding the role of ApoB and Lipoprotein(a) in heart health is only part of the equation—knowing how to test for them and interpret the results is equally important. While these tests aren't part of routine cholesterol screenings, they are becoming more accessible across the United States.
Testing for ApoB and Lipoprotein(a) is simple and involves a standard blood draw. The ApoB test measures the concentration of apolipoprotein B, which is found on all atherogenic particles. This means the test provides a direct count of the harmful particles in your blood.
The Lipoprotein(a) test measures the concentration of Lp(a). Results can be reported in two ways: milligrams per deciliter (mg/dL) or nanomoles per liter (nmol/L). Most U.S. labs use mg/dL, which measures the mass concentration, while nmol/L reflects the actual number of particles.
You can find ApoB testing at independent labs nationwide, often for under $100. For example, LabCorp offers an ApoB test as part of their Complete Heart Health Test, priced at $169.
The timing of these tests largely depends on your personal and family health history. For Lipoprotein(a), medical guidelines suggest a one-time test for individuals at higher risk.
Testing becomes particularly important if you have a family history of early heart disease, especially if close relatives were diagnosed before age 60. The American Heart Association recommends Lp(a) testing for individuals with specific risk factors, such as a family history of high Lp(a), early heart attack or stroke (before age 55 in men or 65 in women), or aortic stenosis.
The National Lipid Association advises considering Lp(a) testing for those with severe primary hyperlipidemia or when evaluating borderline cases for statin therapy. If you have familial hypercholesterolemia, testing is even more critical, as about one-third of individuals with this condition also show elevated Lp(a) levels.
Your doctor may also recommend testing if you have certain lifestyle or health factors, such as a poor diet, obesity, smoking, diabetes, inactivity, or high blood pressure. Since high Lp(a) levels often don't cause symptoms, testing is key to early detection and prevention.
These tests go beyond standard cholesterol panels, offering a more tailored approach to managing cardiovascular health.
Interpreting ApoB and Lp(a) results involves understanding thresholds set by cardiovascular experts. The risk associated with these markers isn't linear—small increases at lower levels have minimal impact, but significantly elevated levels can sharply raise cardiovascular risk.
For Lipoprotein(a), levels of 50 mg/dL (or 125 nmol/L) or higher are considered a critical threshold. At this point, Lp(a) fosters clotting and inflammation, increasing the likelihood of heart attack, stroke, aortic stenosis, and peripheral artery disease.
However, risk increases become more pronounced only at the highest levels, typically within the top 5–10% of the population.
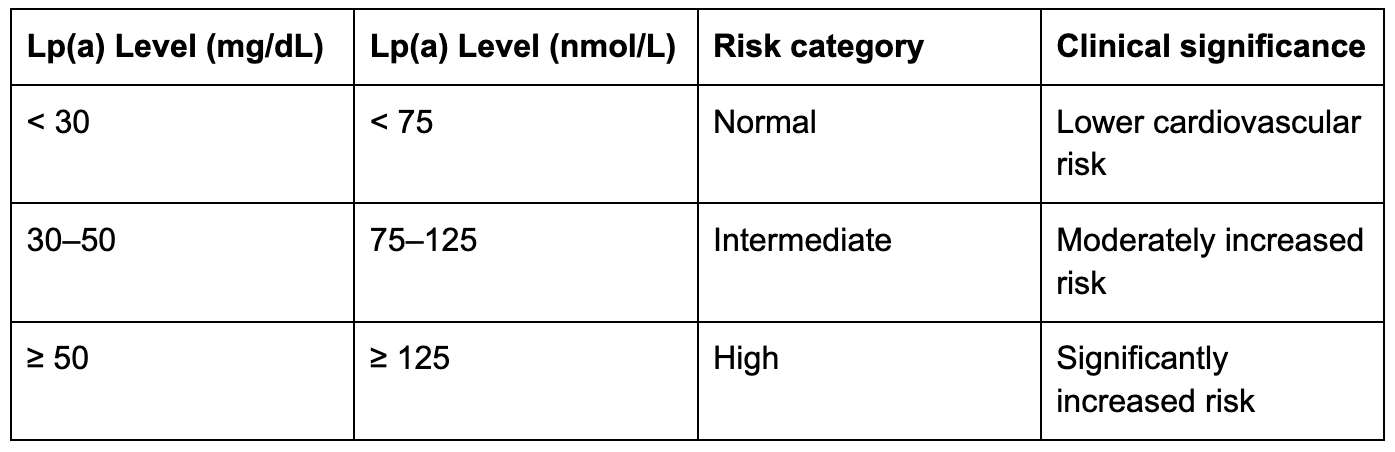
Research shows that Lp(a) values above the 80th percentile (roughly 47 mg/dL) or 90th percentile (43–50 mg/dL) are linked to a substantial rise in cardiovascular disease risk. This highlights the importance of focusing on the upper percentiles when interpreting results.
ApoB testing is especially useful for people with metabolic syndrome or diabetes, as their LDL particles may be smaller and denser. In these cases, ApoB offers a more accurate measure of cardiovascular risk than standard LDL cholesterol levels. While thresholds for ApoB vary, higher levels generally indicate more atherogenic particles in the blood.
About 20–25% of the population has elevated Lp(a) levels. There are also notable racial differences: individuals of African ancestry tend to have significantly higher Lp(a) levels than those of Asian or Caucasian descent. South Asian and Black individuals of African descent often show the highest values.
Your healthcare provider will review your results in the context of your overall health, family history, and risk factors to create a personalised plan for managing your heart health.
Looking for a complete snapshot of your health? Check out our guide on how to get a full body check in Australia to uncover metabolic, thyroid, and longevity insights.
Improving ApoB and Lipoprotein(a) levels requires a mix of targeted lifestyle adjustments and advanced monitoring. While genetics play a significant role in determining Lipoprotein(a) levels, making thoughtful changes to your daily habits can still enhance your overall cardiovascular health.
What you eat can directly affect Lipoprotein(a) levels. Research shows that diets rich in unsaturated fats, like those found in nuts, seeds, and fish, can offer protective benefits. On the flip side, consuming too much saturated fat may increase Lipoprotein(a) levels.
For instance, a study involving 66 women at risk for heart disease found that breakfasts high in polyunsaturated or monounsaturated fats reduced Lipoprotein(a) levels within 30 days. Similarly, snacking on almonds for a month led to a 7.8% drop in Lipoprotein(a) concentration.
Adding heart-friendly foods like flaxseed oil, which may help reduce Lipoprotein(a) gene expression, is another smart choice. A plant-based eating plan focusing on vegetables, fruits, legumes, whole grains, and fish while swapping out saturated and trans fats for unsaturated ones can further improve your lipid profile.
However, individual responses to diet can vary. For example, a 12-week study showed that reducing saturated fat to 6% of total energy intake raised Lipoprotein(a) levels in African American participants, even as their LDL cholesterol decreased.
When it comes to ApoB, regular exercise is key. Unlike Lipoprotein(a), ApoB levels respond well to physical activity. Aerobic exercises like walking, cycling, or swimming, paired with strength training, can help lower ApoB.
The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity each week. Strength training to build muscle and avoiding excess abdominal fat can also contribute to better lipid levels. Losing even 1–2 pounds per week through a balanced diet and consistent exercise can make a difference.
While these efforts address traditional lipid markers, advanced tools like continuous glucose monitoring (CGM) can provide deeper insights into your cardiovascular health.
Advanced lipid markers like ApoB and Lipoprotein(a) can uncover cardiovascular risks that traditional cholesterol tests might miss. But knowing your numbers is only the first step. Understanding how your daily choices affect those risks is what leads to meaningful change. Vively uses continuous glucose monitoring (CGM) and personalised insights to help you improve the metabolic factors that influence heart health.

With Vively, you can
By combining advanced lipid testing with Vively’s real-time metabolic data, you can take a more complete and proactive approach to heart health, addressing both the genetic and lifestyle factors that influence ApoB, Lipoprotein(a), and overall cardiovascular wellbeing.
Lowering Lipoprotein(a) remains a challenge because of its strong genetic ties. While lifestyle changes can only modestly reduce levels, they are still essential for overall heart health. Doctors recommend staying active, eating a balanced diet, avoiding smoking, getting enough sleep, and maintaining a healthy weight.
On the research front, new treatments like antisense oligonucleotides and small interfering RNA therapies are being developed, but they are still in clinical trials. Since pharmaceutical options are limited, regular monitoring is crucial.
Combining advanced tools like CGM with traditional lipid tests creates a more complete approach to heart health, blending immediate metabolic feedback with long-term insights into lipid levels.
Want to understand how thyroid imbalances may be affecting your metabolism? Dive into our guide on understanding thyroid tests—TSH, T3, T4—and what your results mean.
When it comes to understanding your heart health, looking beyond LDL cholesterol is critical. Advanced markers like ApoB and Lipoprotein(a) (Lp(a)) offer a much clearer picture of cardiovascular risk. Studies show that ApoB and Lp(a) are stronger predictors of atherogenic risk compared to LDL-C alone.
For example, a single standard deviation increase in ApoB levels is linked to a 33% higher risk of coronary artery disease. Similarly, elevated Lp(a) levels can significantly increase the chances of heart disease, even when other risk factors are accounted for.
Alarmingly, about 50% of patients who experience recurrent coronary syndrome have normal cholesterol levels based on standard testing. This highlights a major gap in traditional lipid panels, which often miss critical warning signs. Lp(a), in particular, acts as an independent risk factor that promotes clotting and inflammation, making heart attacks and strokes more likely.
Yet, these advanced tests are rarely used. Data shows that only 0.55% of individuals undergoing any lipid testing had an ApoB test, and just 0.37% were tested for Lp(a). This underuse represents a missed opportunity to identify hidden cardiovascular risks early.
Incorporating other tools, like continuous glucose monitoring, alongside lipid testing can provide a more complete picture of your heart health. Together, these insights emphasise the importance of proactive risk management.
Now that you have this information, you can take meaningful steps to protect your heart. Start by discussing ApoB and Lipoprotein(a) testing with your doctor during your next checkup.
Experts recommend that everyone get tested for Lp(a) at least once in their lifetime. If your levels are elevated, it’s essential to screen close family members, as the risk is often genetic. For ApoB, regular blood tests can help you monitor progress after making changes to your diet and lifestyle.
To reduce cardiovascular risk, focus on these key lifestyle habits:
You might also consider adding Vively’s continuous glucose monitoring program to your routine. This tool lets you see how your diet, exercise, and sleep impact your glucose levels in real time, offering valuable insights into your metabolic health that complement traditional lipid testing.
With 20–25% of the global population affected by elevated Lp(a), and many people unaware of their cardiovascular risks, taking proactive steps like advanced testing and monitoring could make a life-saving difference.
ApoB and Lipoprotein(a) offer a clearer understanding of cardiovascular risk because they measure the actual count of harmful lipoprotein particles in your bloodstream. While LDL cholesterol (LDL-C) shows the amount of cholesterol these particles carry, it doesn’t reveal how many particles are present, a critical factor in determining risk.
For instance, even if your LDL-C levels seem normal, having a high number of ApoB particles or elevated Lipoprotein(a) can still signal a serious risk for heart disease. These advanced markers are crucial for uncovering risks that standard LDL-C tests might overlook, empowering you to take proactive steps toward safeguarding your heart health.
If heart disease, high cholesterol, or other cardiovascular concerns run in your family, testing for ApoB and Lipoprotein(a) could offer valuable insights into your heart health. These biomarkers go beyond standard cholesterol tests, providing a more detailed picture of your cardiovascular risk.
Elevated levels of ApoB or Lipoprotein(a) are linked to a higher risk of cardiovascular disease. Should your results come back high, your doctor might suggest changes like adopting a healthier diet, incorporating more exercise, or exploring medical treatments to lower your risk. By testing these markers, you can take a more tailored approach to safeguarding your heart.
Adopting a heart-friendly lifestyle can play a role in improving ApoB and Lipoprotein(a) (Lp(a)) levels to some degree. This means focusing on a diet packed with fruits, vegetables, whole grains, and healthy fats, staying active, keeping a healthy weight, managing stress, quitting smoking, and cutting back on alcohol. These steps not only support your overall heart health but may also help lower ApoB levels slightly.
That said, it's crucial to understand that Lp(a) levels are mostly dictated by genetics, with up to 90% of their variation being inherited. Because of this, lifestyle changes have minimal influence on Lp(a) levels specifically. If you're worried about your heart health, it’s a good idea to talk with your healthcare provider about advanced testing and personalised approaches to better assess and manage these risk factors.
ApoB and Lipoprotein(a) offer a clearer understanding of cardiovascular risk because they measure the actual count of harmful lipoprotein particles in your bloodstream. While LDL cholesterol (LDL-C) shows the amount of cholesterol these particles carry, it doesn’t reveal how many particles are present, a critical factor in determining risk.
For instance, even if your LDL-C levels seem normal, having a high number of ApoB particles or elevated Lipoprotein(a) can still signal a serious risk for heart disease. These advanced markers are crucial for uncovering risks that standard LDL-C tests might overlook, empowering you to take proactive steps toward safeguarding your heart health.
Should I get tested for ApoB and Lipoprotein(a), and what do the results mean for my heart health?
If heart disease, high cholesterol, or other cardiovascular concerns run in your family, testing for ApoB and Lipoprotein(a) could offer valuable insights into your heart health. These biomarkers go beyond standard cholesterol tests, providing a more detailed picture of your cardiovascular risk.
Elevated levels of ApoB or Lipoprotein(a) are linked to a higher risk of cardiovascular disease. Should your results come back high, your doctor might suggest changes like adopting a healthier diet, incorporating more exercise, or exploring medical treatments to lower your risk. By testing these markers, you can take a more tailored approach to safeguarding your heart.
Adopting a heart-friendly lifestyle can play a role in improving ApoB and Lipoprotein(a) (Lp(a)) levels to some degree. This means focusing on a diet packed with fruits, vegetables, whole grains, and healthy fats, staying active, keeping a healthy weight, managing stress, quitting smoking, and cutting back on alcohol. These steps not only support your overall heart health but may also help lower ApoB levels slightly.
That said, it's crucial to understand that Lp(a) levels are mostly dictated by genetics, with up to 90% of their variation being inherited. Because of this, lifestyle changes have minimal influence on Lp(a) levels specifically. If you're worried about your heart health, it’s a good idea to talk with your healthcare provider about advanced testing and personalised approaches to better assess and manage these risk factors.
Subscribe to our newsletter & join a community of 20,000+ Aussies
LDL cholesterol alone isn’t enough to assess your heart health. Many people with normal LDL levels still face heart attacks, while others with high LDL remain unaffected. That’s where ApoB and Lipoprotein(a) (Lp(a)) come in.
These advanced markers provide a clearer picture of cardiovascular risk by focusing on the number of harmful particles in your blood and genetic factors that standard tests miss.
Talk to your doctor about these tests and take control of your heart health by combining advanced lipid testing with healthy lifestyle choices.
ApoB and Lipoprotein(a) provide insights that go beyond what traditional cholesterol tests can reveal. While standard cholesterol measurements focus on the amount of cholesterol in the blood, these markers shed light on the number of atherogenic particles and highlight genetic factors that influence cardiovascular risk.
Let’s break down how each of these markers plays a role in heart disease and increases risk.
ApoB (apolipoprotein B) is a crucial structural protein found in all atherogenic lipoproteins. It comes in two forms ApoB48 and ApoB100 with ApoB100 being the one most relevant to heart health. Produced in the liver, ApoB100 is present on lipoproteins like VLDL, IDL, and LDL. Each atherogenic particle carries exactly one ApoB molecule, meaning the concentration of ApoB directly reflects the number of harmful particles in the bloodstream. When these particles get trapped in arterial walls, they spark inflammation and plaque buildup, significantly raising the risk of heart attacks.
Interestingly, ApoB and LDL cholesterol levels don’t always align. Research shows that in about 20% of patients, especially those with high triglycerides, type 2 diabetes, or obesity, ApoB levels can be elevated even when LDL cholesterol appears normal. This means someone with "healthy" LDL cholesterol might still face a heightened risk of heart disease if their ApoB levels are high.
Lipoprotein(a), often abbreviated as Lp(a), adds a unique layer of risk due to its strong genetic component. Lp(a) consists of an LDL particle attached to an additional protein called apolipoprotein(a). Genetics determine 70% to 90% of Lp(a) levels, so lifestyle changes have little impact on reducing its concentration.
Unlike LDL, Lp(a) not only contributes to plaque buildup but also promotes blood clotting and inflammation. This combination increases the risk of heart attack, stroke, aortic valve narrowing, and peripheral artery disease. Levels of Lp(a) above 50 mg/dL (125 nmol/L) are linked to a significantly higher risk of cardiovascular events.
Certain groups, such as individuals of African descent or South Asian heritage, tend to have higher average Lp(a) levels. Additionally, a genetic variation called the KIV2 copy number variant explains much of the variability in Lp(a) levels between individuals.
Studies consistently show that ApoB and Lp(a) are better predictors of cardiovascular risk than traditional cholesterol measurements. A systematic review found that ApoB outperformed LDL cholesterol in predicting cardiovascular events across all studies analyzed.
Similarly, a meta-analysis published in The Lancet highlighted that counting atherogenic particles via ApoB offers a clearer picture of risk compared to focusing solely on the cholesterol content in LDL or non-HDL particles.
For Lp(a), data from the UK Biobank cohort revealed that its association with cardiovascular disease risk is over six times stronger than that of LDL particles. Globally, elevated Lp(a) levels affect more than 1.5 billion people and are linked to a 31% higher risk of cardiovascular disease and a 42% greater chance of an atherosclerotic event.
Even when LDL cholesterol is well-controlled, Lp(a) remains an independent risk factor, with cardiovascular risk rising by 11% for every 50 nmol/L increase in Lp(a). At concentrations above 180 mg/dL, Lp(a)-related cardiovascular risk mirrors that seen in patients with heterozygous familial hypercholesterolemia.
These findings highlight why measuring ApoB and Lp(a) during routine cardiovascular evaluations can provide a more complete understanding of heart disease risk.
Want to know which tests can help you live healthier for longer? Read our guide on the top five longevity biomarkers and how they can guide your health decisions.
Understanding the role of ApoB and Lipoprotein(a) in heart health is only part of the equation—knowing how to test for them and interpret the results is equally important. While these tests aren't part of routine cholesterol screenings, they are becoming more accessible across the United States.
Testing for ApoB and Lipoprotein(a) is simple and involves a standard blood draw. The ApoB test measures the concentration of apolipoprotein B, which is found on all atherogenic particles. This means the test provides a direct count of the harmful particles in your blood.
The Lipoprotein(a) test measures the concentration of Lp(a). Results can be reported in two ways: milligrams per deciliter (mg/dL) or nanomoles per liter (nmol/L). Most U.S. labs use mg/dL, which measures the mass concentration, while nmol/L reflects the actual number of particles.
You can find ApoB testing at independent labs nationwide, often for under $100. For example, LabCorp offers an ApoB test as part of their Complete Heart Health Test, priced at $169.
The timing of these tests largely depends on your personal and family health history. For Lipoprotein(a), medical guidelines suggest a one-time test for individuals at higher risk.
Testing becomes particularly important if you have a family history of early heart disease, especially if close relatives were diagnosed before age 60. The American Heart Association recommends Lp(a) testing for individuals with specific risk factors, such as a family history of high Lp(a), early heart attack or stroke (before age 55 in men or 65 in women), or aortic stenosis.
The National Lipid Association advises considering Lp(a) testing for those with severe primary hyperlipidemia or when evaluating borderline cases for statin therapy. If you have familial hypercholesterolemia, testing is even more critical, as about one-third of individuals with this condition also show elevated Lp(a) levels.
Your doctor may also recommend testing if you have certain lifestyle or health factors, such as a poor diet, obesity, smoking, diabetes, inactivity, or high blood pressure. Since high Lp(a) levels often don't cause symptoms, testing is key to early detection and prevention.
These tests go beyond standard cholesterol panels, offering a more tailored approach to managing cardiovascular health.
Interpreting ApoB and Lp(a) results involves understanding thresholds set by cardiovascular experts. The risk associated with these markers isn't linear—small increases at lower levels have minimal impact, but significantly elevated levels can sharply raise cardiovascular risk.
For Lipoprotein(a), levels of 50 mg/dL (or 125 nmol/L) or higher are considered a critical threshold. At this point, Lp(a) fosters clotting and inflammation, increasing the likelihood of heart attack, stroke, aortic stenosis, and peripheral artery disease.
However, risk increases become more pronounced only at the highest levels, typically within the top 5–10% of the population.
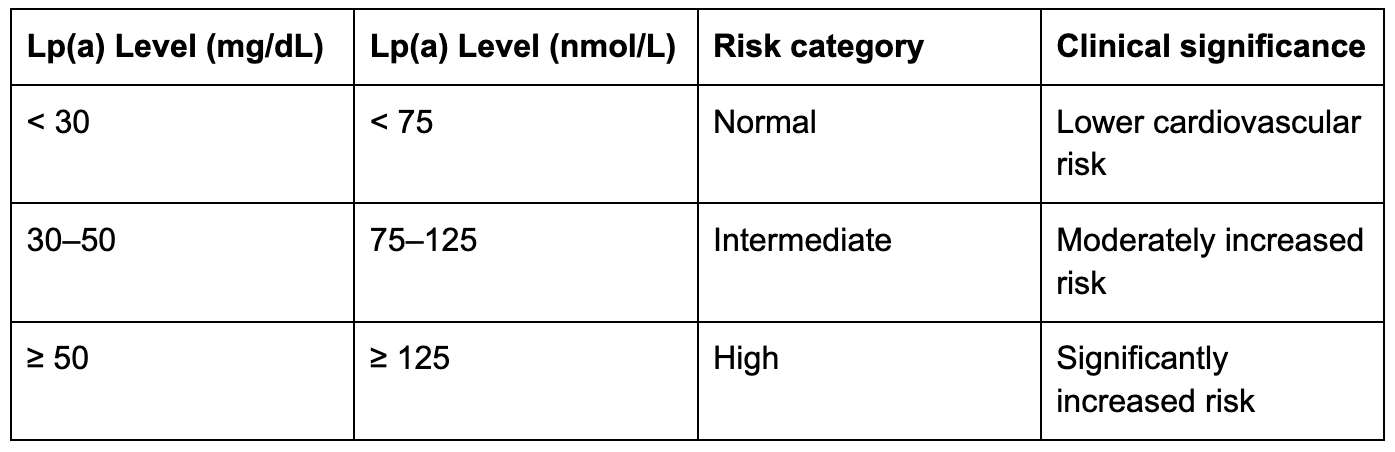
Research shows that Lp(a) values above the 80th percentile (roughly 47 mg/dL) or 90th percentile (43–50 mg/dL) are linked to a substantial rise in cardiovascular disease risk. This highlights the importance of focusing on the upper percentiles when interpreting results.
ApoB testing is especially useful for people with metabolic syndrome or diabetes, as their LDL particles may be smaller and denser. In these cases, ApoB offers a more accurate measure of cardiovascular risk than standard LDL cholesterol levels. While thresholds for ApoB vary, higher levels generally indicate more atherogenic particles in the blood.
About 20–25% of the population has elevated Lp(a) levels. There are also notable racial differences: individuals of African ancestry tend to have significantly higher Lp(a) levels than those of Asian or Caucasian descent. South Asian and Black individuals of African descent often show the highest values.
Your healthcare provider will review your results in the context of your overall health, family history, and risk factors to create a personalised plan for managing your heart health.
Looking for a complete snapshot of your health? Check out our guide on how to get a full body check in Australia to uncover metabolic, thyroid, and longevity insights.
Improving ApoB and Lipoprotein(a) levels requires a mix of targeted lifestyle adjustments and advanced monitoring. While genetics play a significant role in determining Lipoprotein(a) levels, making thoughtful changes to your daily habits can still enhance your overall cardiovascular health.
What you eat can directly affect Lipoprotein(a) levels. Research shows that diets rich in unsaturated fats, like those found in nuts, seeds, and fish, can offer protective benefits. On the flip side, consuming too much saturated fat may increase Lipoprotein(a) levels.
For instance, a study involving 66 women at risk for heart disease found that breakfasts high in polyunsaturated or monounsaturated fats reduced Lipoprotein(a) levels within 30 days. Similarly, snacking on almonds for a month led to a 7.8% drop in Lipoprotein(a) concentration.
Adding heart-friendly foods like flaxseed oil, which may help reduce Lipoprotein(a) gene expression, is another smart choice. A plant-based eating plan focusing on vegetables, fruits, legumes, whole grains, and fish while swapping out saturated and trans fats for unsaturated ones can further improve your lipid profile.
However, individual responses to diet can vary. For example, a 12-week study showed that reducing saturated fat to 6% of total energy intake raised Lipoprotein(a) levels in African American participants, even as their LDL cholesterol decreased.
When it comes to ApoB, regular exercise is key. Unlike Lipoprotein(a), ApoB levels respond well to physical activity. Aerobic exercises like walking, cycling, or swimming, paired with strength training, can help lower ApoB.
The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity each week. Strength training to build muscle and avoiding excess abdominal fat can also contribute to better lipid levels. Losing even 1–2 pounds per week through a balanced diet and consistent exercise can make a difference.
While these efforts address traditional lipid markers, advanced tools like continuous glucose monitoring (CGM) can provide deeper insights into your cardiovascular health.
Advanced lipid markers like ApoB and Lipoprotein(a) can uncover cardiovascular risks that traditional cholesterol tests might miss. But knowing your numbers is only the first step. Understanding how your daily choices affect those risks is what leads to meaningful change. Vively uses continuous glucose monitoring (CGM) and personalised insights to help you improve the metabolic factors that influence heart health.

With Vively, you can
By combining advanced lipid testing with Vively’s real-time metabolic data, you can take a more complete and proactive approach to heart health, addressing both the genetic and lifestyle factors that influence ApoB, Lipoprotein(a), and overall cardiovascular wellbeing.
Lowering Lipoprotein(a) remains a challenge because of its strong genetic ties. While lifestyle changes can only modestly reduce levels, they are still essential for overall heart health. Doctors recommend staying active, eating a balanced diet, avoiding smoking, getting enough sleep, and maintaining a healthy weight.
On the research front, new treatments like antisense oligonucleotides and small interfering RNA therapies are being developed, but they are still in clinical trials. Since pharmaceutical options are limited, regular monitoring is crucial.
Combining advanced tools like CGM with traditional lipid tests creates a more complete approach to heart health, blending immediate metabolic feedback with long-term insights into lipid levels.
Want to understand how thyroid imbalances may be affecting your metabolism? Dive into our guide on understanding thyroid tests—TSH, T3, T4—and what your results mean.
When it comes to understanding your heart health, looking beyond LDL cholesterol is critical. Advanced markers like ApoB and Lipoprotein(a) (Lp(a)) offer a much clearer picture of cardiovascular risk. Studies show that ApoB and Lp(a) are stronger predictors of atherogenic risk compared to LDL-C alone.
For example, a single standard deviation increase in ApoB levels is linked to a 33% higher risk of coronary artery disease. Similarly, elevated Lp(a) levels can significantly increase the chances of heart disease, even when other risk factors are accounted for.
Alarmingly, about 50% of patients who experience recurrent coronary syndrome have normal cholesterol levels based on standard testing. This highlights a major gap in traditional lipid panels, which often miss critical warning signs. Lp(a), in particular, acts as an independent risk factor that promotes clotting and inflammation, making heart attacks and strokes more likely.
Yet, these advanced tests are rarely used. Data shows that only 0.55% of individuals undergoing any lipid testing had an ApoB test, and just 0.37% were tested for Lp(a). This underuse represents a missed opportunity to identify hidden cardiovascular risks early.
Incorporating other tools, like continuous glucose monitoring, alongside lipid testing can provide a more complete picture of your heart health. Together, these insights emphasise the importance of proactive risk management.
Now that you have this information, you can take meaningful steps to protect your heart. Start by discussing ApoB and Lipoprotein(a) testing with your doctor during your next checkup.
Experts recommend that everyone get tested for Lp(a) at least once in their lifetime. If your levels are elevated, it’s essential to screen close family members, as the risk is often genetic. For ApoB, regular blood tests can help you monitor progress after making changes to your diet and lifestyle.
To reduce cardiovascular risk, focus on these key lifestyle habits:
You might also consider adding Vively’s continuous glucose monitoring program to your routine. This tool lets you see how your diet, exercise, and sleep impact your glucose levels in real time, offering valuable insights into your metabolic health that complement traditional lipid testing.
With 20–25% of the global population affected by elevated Lp(a), and many people unaware of their cardiovascular risks, taking proactive steps like advanced testing and monitoring could make a life-saving difference.
ApoB and Lipoprotein(a) offer a clearer understanding of cardiovascular risk because they measure the actual count of harmful lipoprotein particles in your bloodstream. While LDL cholesterol (LDL-C) shows the amount of cholesterol these particles carry, it doesn’t reveal how many particles are present, a critical factor in determining risk.
For instance, even if your LDL-C levels seem normal, having a high number of ApoB particles or elevated Lipoprotein(a) can still signal a serious risk for heart disease. These advanced markers are crucial for uncovering risks that standard LDL-C tests might overlook, empowering you to take proactive steps toward safeguarding your heart health.
If heart disease, high cholesterol, or other cardiovascular concerns run in your family, testing for ApoB and Lipoprotein(a) could offer valuable insights into your heart health. These biomarkers go beyond standard cholesterol tests, providing a more detailed picture of your cardiovascular risk.
Elevated levels of ApoB or Lipoprotein(a) are linked to a higher risk of cardiovascular disease. Should your results come back high, your doctor might suggest changes like adopting a healthier diet, incorporating more exercise, or exploring medical treatments to lower your risk. By testing these markers, you can take a more tailored approach to safeguarding your heart.
Adopting a heart-friendly lifestyle can play a role in improving ApoB and Lipoprotein(a) (Lp(a)) levels to some degree. This means focusing on a diet packed with fruits, vegetables, whole grains, and healthy fats, staying active, keeping a healthy weight, managing stress, quitting smoking, and cutting back on alcohol. These steps not only support your overall heart health but may also help lower ApoB levels slightly.
That said, it's crucial to understand that Lp(a) levels are mostly dictated by genetics, with up to 90% of their variation being inherited. Because of this, lifestyle changes have minimal influence on Lp(a) levels specifically. If you're worried about your heart health, it’s a good idea to talk with your healthcare provider about advanced testing and personalised approaches to better assess and manage these risk factors.
ApoB and Lipoprotein(a) offer a clearer understanding of cardiovascular risk because they measure the actual count of harmful lipoprotein particles in your bloodstream. While LDL cholesterol (LDL-C) shows the amount of cholesterol these particles carry, it doesn’t reveal how many particles are present, a critical factor in determining risk.
For instance, even if your LDL-C levels seem normal, having a high number of ApoB particles or elevated Lipoprotein(a) can still signal a serious risk for heart disease. These advanced markers are crucial for uncovering risks that standard LDL-C tests might overlook, empowering you to take proactive steps toward safeguarding your heart health.
Should I get tested for ApoB and Lipoprotein(a), and what do the results mean for my heart health?
If heart disease, high cholesterol, or other cardiovascular concerns run in your family, testing for ApoB and Lipoprotein(a) could offer valuable insights into your heart health. These biomarkers go beyond standard cholesterol tests, providing a more detailed picture of your cardiovascular risk.
Elevated levels of ApoB or Lipoprotein(a) are linked to a higher risk of cardiovascular disease. Should your results come back high, your doctor might suggest changes like adopting a healthier diet, incorporating more exercise, or exploring medical treatments to lower your risk. By testing these markers, you can take a more tailored approach to safeguarding your heart.
Adopting a heart-friendly lifestyle can play a role in improving ApoB and Lipoprotein(a) (Lp(a)) levels to some degree. This means focusing on a diet packed with fruits, vegetables, whole grains, and healthy fats, staying active, keeping a healthy weight, managing stress, quitting smoking, and cutting back on alcohol. These steps not only support your overall heart health but may also help lower ApoB levels slightly.
That said, it's crucial to understand that Lp(a) levels are mostly dictated by genetics, with up to 90% of their variation being inherited. Because of this, lifestyle changes have minimal influence on Lp(a) levels specifically. If you're worried about your heart health, it’s a good idea to talk with your healthcare provider about advanced testing and personalised approaches to better assess and manage these risk factors.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
