New Launch - Try our Next-Gen Glucose Monitoring Program
Choose how you’d like to begin
CGM program
Optimise metabolism in real time with sensors

Advanced Blood Test
Get your baseline health report and personalised plan



Discover the underlying causes and effective management strategies for menopause joint pain and muscle aches. Understand how factors like weight gain, inflammation, sleep issues, and mental health can influence pain during the menopausal transition and what you can do about it.
The menopausal transition can be a challenging time for women, with approximately 70-80% experiencing musculoskeletal pain. This pain presents itself in various forms, including muscle aches, joint pains, fatigue, tendon inflammation, and increased soft-tissue injury.
The exact mechanisms causing these joint aches and pains are not fully understood, but several associated conditions can help to explain this complex process. This article aims to take an in-depth look at the causes and solutions for menopause joint and muscle pain.
Women carrying excess weight, particularly those with a body mass index (BMI) over 30, are more likely to experience new onset pain during menopause. The key reason for this is the increase in inflammatory chemicals produced by fat cells.
Oestrogen, which significantly reduces during menopause, is known to modulate key inflammatory chemicals, called cytokines. As oestrogen levels decline, inflammatory impacts increase due to a rise in cytokines like Interleukin-6 (IL-6), Interleukin 12 (IL12), and Tumour Necrosis Factor alpha (TNF α). These cytokines are produced within adipocytes (fat cells), which are now known to be metabolically active and responsible for producing reactive chemicals.
The more fat mass one carries, the more inflammation is likely to occur, and the drop in oestrogen may catalyse these changes. Changes in insulin sensitivity further exacerbate the inflammatory cascade, increasing the risk of abdominal fat deposition. Reversing this cycle, especially in the early stages of menopausal transition, is crucial.
Hormone level changes during the peri-menopausal stage can lead to shifts in body mass, fat mass, and fat distribution. These changes can adversely affect muscle health, energy, and metabolism. Furthermore, if a woman begins to experience menopause joint pain, it may make maintaining a healthy exercise regime challenging, potentially initiating a vicious cycle.
Sleep plays a vital role in managing pain perception. As oestrogen and progesterone levels decrease during menopause, sleep disturbances become a common complaint. The reciprocal relationship between poor sleep and increased pain can lead to a damaging cycle.
This is where poor sleep, driven by worsening mental health, hot flushes, night sweats, glucose dysregulation or excessive pain, negatively impacts the quality of sleep, leading to even more pain and disruptions. Optimising sleep through hormone replacement, complementary medicines, non-hormonal options or lifestyle interventions is crucial. These strategies can modify pain perception and potentially reduce inflammation.
During menopause, significant hormonal changes can lead to mood alterations, with increased irritability, anxiety, and depression frequently observed. These shifts in mental health are not just distressing emotionally but can have a profound effect on the physical body, particularly on the perception and severity of pain.
Depression has long been associated with an increase in pain perception and severity, however the research is variable and may depend on the kind of pain being experienced. Looking at optimising both physical and mental conditioning may help to manage the changes in pain and inflammation during menopause. More research is needed to fully understand this concept.
The exact mechanism for the increased prevalence of musculoskeletal issues during menopause remains uncertain. However, addressing lifestyle factors such as managing sleep, maintaining a healthy exercise regime, regulating glucose variability and reducing inflammatory foods can make a difference for women who experience joint pain.
In addition, consulting with a healthcare professional regarding sleep, pain management and hormone replacement options can provide invaluable guidance. Understanding the unique interplay of factors during this time can guide you in making healthier choices and treatment decisions.
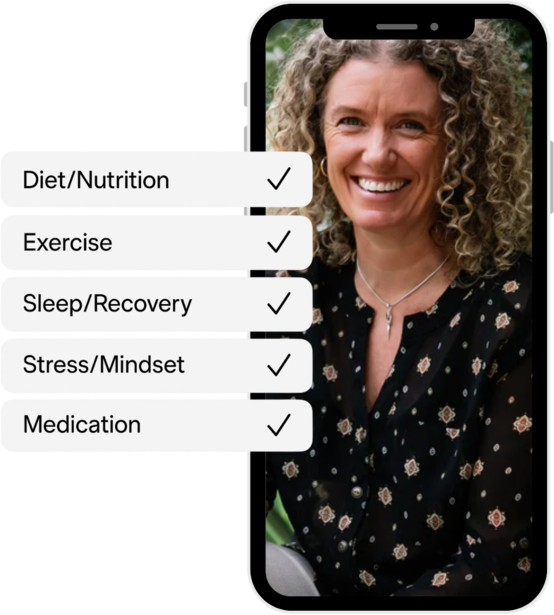
A resource such as Vively, can assist in managing some of these aspects. Vively can help improve glucose control, contributing to better sleep, mood regulation, and overall well-being. By helping to break the cycle of poor sleep and glucose dysregulation, Vively can play a part in managing menopause joint pain and ensuring a healthier menopausal transition.
Subscribe to our newsletter & join a community of 20,000+ Aussies

Discover the underlying causes and effective management strategies for menopause joint pain and muscle aches. Understand how factors like weight gain, inflammation, sleep issues, and mental health can influence pain during the menopausal transition and what you can do about it.
The menopausal transition can be a challenging time for women, with approximately 70-80% experiencing musculoskeletal pain. This pain presents itself in various forms, including muscle aches, joint pains, fatigue, tendon inflammation, and increased soft-tissue injury.
The exact mechanisms causing these joint aches and pains are not fully understood, but several associated conditions can help to explain this complex process. This article aims to take an in-depth look at the causes and solutions for menopause joint and muscle pain.
Women carrying excess weight, particularly those with a body mass index (BMI) over 30, are more likely to experience new onset pain during menopause. The key reason for this is the increase in inflammatory chemicals produced by fat cells.
Oestrogen, which significantly reduces during menopause, is known to modulate key inflammatory chemicals, called cytokines. As oestrogen levels decline, inflammatory impacts increase due to a rise in cytokines like Interleukin-6 (IL-6), Interleukin 12 (IL12), and Tumour Necrosis Factor alpha (TNF α). These cytokines are produced within adipocytes (fat cells), which are now known to be metabolically active and responsible for producing reactive chemicals.
The more fat mass one carries, the more inflammation is likely to occur, and the drop in oestrogen may catalyse these changes. Changes in insulin sensitivity further exacerbate the inflammatory cascade, increasing the risk of abdominal fat deposition. Reversing this cycle, especially in the early stages of menopausal transition, is crucial.
Hormone level changes during the peri-menopausal stage can lead to shifts in body mass, fat mass, and fat distribution. These changes can adversely affect muscle health, energy, and metabolism. Furthermore, if a woman begins to experience menopause joint pain, it may make maintaining a healthy exercise regime challenging, potentially initiating a vicious cycle.
Sleep plays a vital role in managing pain perception. As oestrogen and progesterone levels decrease during menopause, sleep disturbances become a common complaint. The reciprocal relationship between poor sleep and increased pain can lead to a damaging cycle.
This is where poor sleep, driven by worsening mental health, hot flushes, night sweats, glucose dysregulation or excessive pain, negatively impacts the quality of sleep, leading to even more pain and disruptions. Optimising sleep through hormone replacement, complementary medicines, non-hormonal options or lifestyle interventions is crucial. These strategies can modify pain perception and potentially reduce inflammation.
During menopause, significant hormonal changes can lead to mood alterations, with increased irritability, anxiety, and depression frequently observed. These shifts in mental health are not just distressing emotionally but can have a profound effect on the physical body, particularly on the perception and severity of pain.
Depression has long been associated with an increase in pain perception and severity, however the research is variable and may depend on the kind of pain being experienced. Looking at optimising both physical and mental conditioning may help to manage the changes in pain and inflammation during menopause. More research is needed to fully understand this concept.
The exact mechanism for the increased prevalence of musculoskeletal issues during menopause remains uncertain. However, addressing lifestyle factors such as managing sleep, maintaining a healthy exercise regime, regulating glucose variability and reducing inflammatory foods can make a difference for women who experience joint pain.
In addition, consulting with a healthcare professional regarding sleep, pain management and hormone replacement options can provide invaluable guidance. Understanding the unique interplay of factors during this time can guide you in making healthier choices and treatment decisions.
A resource such as Vively, can assist in managing some of these aspects. Vively can help improve glucose control, contributing to better sleep, mood regulation, and overall well-being. By helping to break the cycle of poor sleep and glucose dysregulation, Vively can play a part in managing menopause joint pain and ensuring a healthier menopausal transition.
Get irrefutable data about your diet and lifestyle by using your own glucose data with Vively’s CGM Program. We’re currently offering a 20% discount for our annual plan. Sign up here.

Discover how controlling your glucose levels can aid in ageing gracefully. Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well.


Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices. Learn about practical strategies to implement mindful eating in your daily life.


Understand the nuances of polycystic ovary syndrome (PCOS) testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition. Also, find out when these diagnostic procedures should be considered.
